我的设计我做主:MedSci临床研究方案设计活动(第二轮)-立题公布(1)
2015-07-08 MedSci MedSci原创
任务目标:完成一份辅助生殖相关的临床研究设计 在发布的立题选项中,看下方 任务一(2015.7.6发布):临床研究立题(方向) 请各位从以下研究立题中选择一个,开展后续的研究设计任务: A. 卵巢低反应对于IVF妊娠结局的影响 B. OHSS发生的相关风险因素 C. XX激素水平(或者其他biomarker指标)是否可以预测IVF妊娠结局 D. 两种促排方
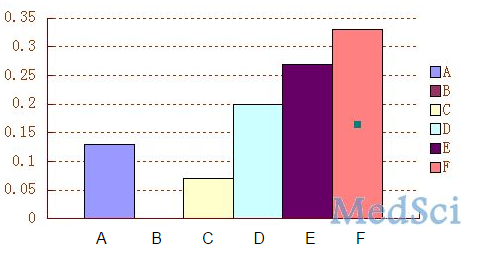
经过统计发现更多的老师选择了F选项,即“二甲双胍是否有助于改善PCOS患者的IVF结局(或者对于二甲双胍相关治疗方案优化的研究)”。紧随其后的是E选项,即“对于肥胖或体重超标者实施体重控制或干预(减轻体重)对于IVF妊娠结局的影响”。
我们非常认同各位的选择,确实这些研究方向是目前辅助生殖相关研究的热点,那么今天我在这里与大家分享一下关于这几个立题的“完善、细化”的建议,并提供一些相关的信息,供大家参考。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













赞
174
#研究方案#
82
#方案设计#
78
不对,看错了…
141
二甲双胍是否有助于改善PCOS患者的IVF,国外已经有注册了。
51
#Med#
54
看看
113
继续学习
131
继续学习
168
等待揭晓
113