Nat Commun:可怕!这些基因竟会影响社交!或是孤独症的罪魁祸首!
2018-07-06 Ruthy,Zoe 转化医学网
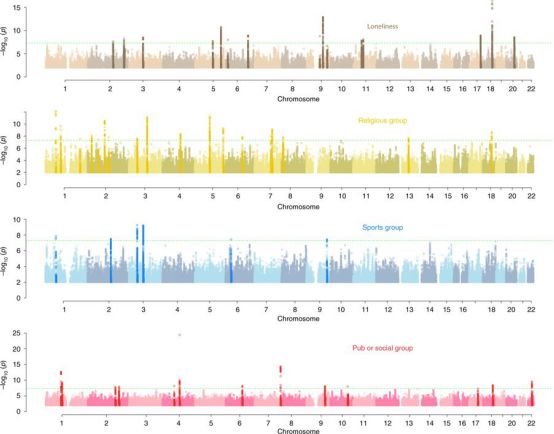
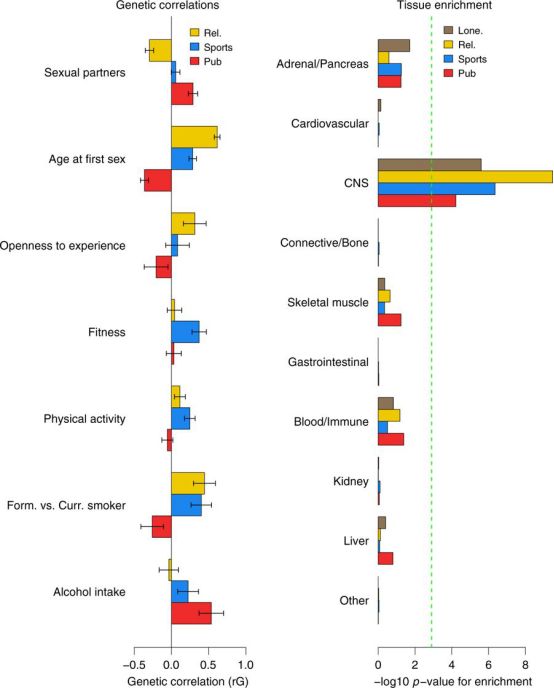
孤独症(又称自闭症)是一种先天性神经系统疾病,临床表现包括社会交往沟通能力障碍、语言发育障碍、兴趣爱好比较狭窄、智能较差、行为活动刻板等。虽然孤独症的病因还不完全清楚,但目前的研究表明,遗传、感染与免疫和孕期理化因子刺激可能同孤独症的发病相关。有研究显示孤独症是一种多基因遗传病,但目前尚未有具体研究揭示孤独症的具体遗传因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
69
#COMMUN#
83
学习了.谢谢分享
140
#社交#
92
了解一下.谢谢分享!
141
学习了
160