病例分享:慢性髓系白血病双费城染色体阳性同时表达P210BCR-ABL1和P195BCR-ABL1
2019-02-16 月下荷花 肿瘤资讯
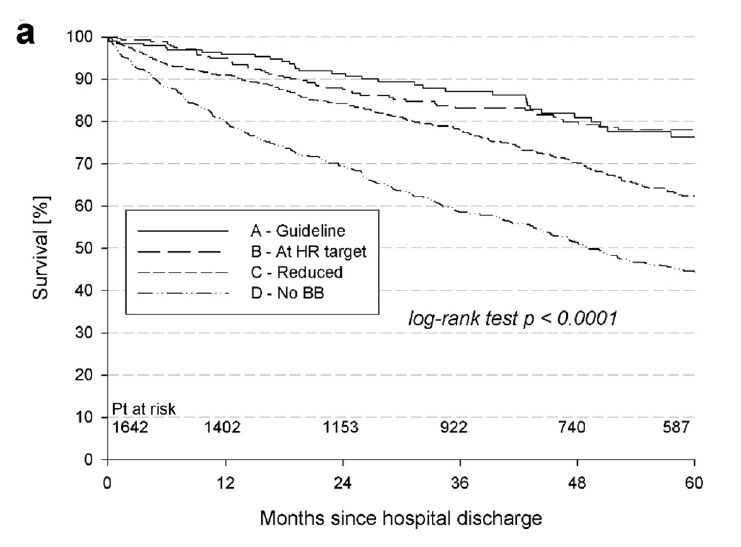
费城染色体[Ph;t(9;22)(q34;q11)]和BCR-ABL1基因是慢性髓系白血病(CML)的标志,大部分CML表达P210BCR-ABL1蛋白,由e14a2或e13a2融合转录产生,5%CML表达少见异构体,包括P190(e1a2)、P195(e6a2)、P200(e8a2)、P225(e18a2)和P230(e19a2),所有异构体均有致病作用,同时也是CML的治疗靶点。Vinhas医


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#髓系白血病#
55
#BCR-ABL1#
67
#p21#
66
#染色体#
42
#费城染色体#
54
#慢性髓系白血病#
52