JACC:大样本研究显示先心病外科术后远期死亡率仍居高不下
2018-05-26 MedSci MedSci原创
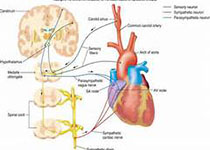
先天性心脏病外科手术治疗能明显提高复杂先心病的生存率,但其远期的预后效果尚未阐明。本研究纳入了美国儿童心脏病数据库中的35998名接受了首次先心病外科手术治疗且存活下来的年龄小于21岁的患者,经过平均18年时间的随访,有3191名患者出现了死亡,标准化死亡率(SMR)为8.3(95% [CI]: 8.0 - 8.7),15年的SMR从早期的12.7(1982-1992)下降至晚期的10(1998-
先天性心脏病外科手术治疗能明显提高复杂先心病的生存率,但其远期的预后效果尚未阐明。本研究纳入了美国儿童心脏病数据库中的35998名接受了首次先心病外科手术治疗且存活下来的年龄小于21岁的患者,经过平均18年时间的随访,有3191名患者出现了死亡,标准化死亡率(SMR)为8.3(95% [CI]: 8.0 - 8.7),15年的SMR从早期的12.7(1982-1992)下降至晚期的10(1998-2003),即使在非严重的先心病患者如动脉导管未闭和房间隔缺损,SMR依旧处于较高水平,而SMR降低最明显的疾病是大动脉转位(11.0 vs 3.8;p<0.05)、完全性房室通道(31.3 vs 15.3; p<0.05)和单心室(53.7vs 37.3;p<0.05)。研究结果显示,各种类型的先天性心脏病外科术后的远期死亡率均较高,对于某些复杂的先心病,患者的远期死亡率逐年下降,但仍处于较高水平。原始出处:Logan G et al.Trends in Long-Term Mortality After Congenital Heart Surgery.JACC.2018 May.本文系梅
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
59
#样本#
52
#先心病#
77
#ACC#
53
很好的学习机会
91
学习了受益匪浅
78
谢谢分享学习
98