Cell:揭示COVID-19无症状或恢复期患者均有强大抵抗力
2020-08-17 张佳兴 生物探索
截止2020年8月17日,新型冠状病毒已给全球造成了巨大的影响,新型冠状病毒肺炎确诊病例高达2159万,死亡病例77万。然而,部分患者在COVID-19期间仅受到较轻的影响,表现为无症状或者轻微症状。
截止到2020年8月17日,新型冠状病毒(SARS-CoV-2)已给全球造成了巨大的影响,新型冠状病毒肺炎(新冠肺炎,COVID-19)确诊病例高达2159万,死亡病例77万。然而,部分患者在COVID-19期间仅受到较轻的影响,表现为无症状或者只出现轻微的症状。
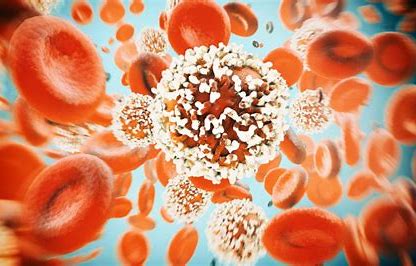
2020年8月14号,瑞典卡罗林斯卡医学院传染病医学中心的研究人员在Cell在线发表题为Robust T cell immunity in convalescent individuals withasymptomatic or mild COVID-19的研究论文,研究发现COVID-19急性期SARS-CoV-2特异性T细胞表现出活化的细胞毒性表型,恢复期呈广泛且多功能的T细胞反应,并且在血清阴性个体中也检测到了SARS-CoV-2特异性T细胞反应。
此前的研究表明,恒河猴中SARS-CoV-2感染可产生保护作用,使其免受二次攻击。同样,新冠肺炎患者再次感染的情况也相对较少。为了评估由SARS-CoV-2初次感染引起的保护性免疫反应的持久性,研究人员招募了206例不同程度的新冠肺炎患者,对其CD4+、CD8+T细胞进行研究。
初步分析表明,急性中、重度新冠肺炎患者CD4+和CD8+T细胞水平较低。PCA分析显示,急性中、重度新冠肺炎患者的记忆T细胞与恢复期患者和健康对照者的记忆T细胞之间有明显的分离,主要表现为CD4+T细胞中CD38、CD69、Ki-67和PD-1的表达以及CD8+T细胞中CD38、CD39、CD69、CTLA-4、HLA-DR、Ki-67、LAG-3和TIM-3的表达。急性中、重度新冠肺炎患者的记忆CD4+T和CD8+T细胞高表达与激活和细胞周期相关的标志物。进一步的相关性分析表明,激活和细胞周期相关的标志物的表达与SARS-CoV-2 IgG水平以及各种临床参数密切相关。这些结果表明,COVID-19早期机体具有强大的SARS-COV-2特异性免疫反应。
进一步分析中,研究人员发现,与恢复期和健康对照者相比,急性中、重度新冠肺炎患者的记忆CD8+T细胞高表达CD38,在SARS-CoV-2特异性CD8+T细胞中,CCR7和CD45RA的表达与感染后无症状天数呈正相关,而颗粒酶B的表达则呈负相关。
于是,研究人员量化了不同队列中的功能性SARS-CoV2特异性记忆T细胞反应,包括大流行前采血的健康对照,新冠肺炎患者的家庭成员,以及新冠肺炎轻、重度感染后处于恢复期的患者。研究发现,新冠肺炎恢复期的患者,均出现对SARS-CoV2棘蛋白、膜蛋白和核衣壳蛋白的T细胞反应。
SARS-CoV-2特异性CD4+T细胞主要表达IFN-γ、IL-2和TNF,而SARS-CoV-2特异性CD8+T细胞主要表达IFN-γ。有趣的是,棘蛋白特异性的CD4+T细胞向T滤泡辅助细胞极化,而膜特异性和核衣壳特异性的CD4+T细胞向Th1或Th1/Th17极化。
最后,研究人员发现大多数恢复期患者和暴露的家庭成员均能检测到记忆CD4+和CD8+T细胞。血清学评价显示,针对SARS-CoV2棘蛋白的免疫球蛋白反应与针对SARS-CoV2核衣壳蛋白的免疫球蛋白反应呈高度正相关。与未暴露的健康对照相比,血清阴性的家庭成员的T细胞反应也更强。因此,在没有或存在循环抗体的情况下,机体可以激发强有力的记忆T细胞反应。
总之,该研究系统分析了暴露、感染和疾病全过程中SARS-CoV-2特异性T细胞免疫的功能和表型图谱,发现许多无症状或轻度新冠肺炎患者在接触或感染SARS-CoV-2后,产生了高度持久和功能丰富的记忆T细胞反应,并且自然暴露或感染可以防止重症新冠肺炎复发。
原始出处:
Takuya Sekine,André Perez-Potti,Olga Rivera-Ballesteros,et al.Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19.cell.Open AccessPublished:August 14, 2020DOI:https://doi.org/10.1016/j.cell.2020.08.017
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#恢复期#
78
#CEL#
59
#Cell#
75
👍🏻
170
#无症状#
69
#抵抗力#
89
好
118