“人类多动一小步,痴呆退后一大步!”轻量运动即使痴呆风险打5折!大量运动最多推迟12年!
2021-12-12 LILYMED MedSci原创
BMC Med.:设备测量的身体活动与痴呆发病之间的剂量-反应相关性:英国生物库的一项前瞻性研究
身体活动(PA)被公认与几种健康益处有关,并能降低整个生命周期中不良健康结果的风险。 事实上,世界卫生组织(WHO)于2020年发布的《身体活动和久坐行为指南》强调,"每一步都很重要"。根据这些指南,成人应每周至少进行150-300分钟的中度PA(或每周75-150分钟的剧烈PA或相当于每周至少600次代谢当量任务[MET]/min的中度至剧烈PA [MVPA])。然而,据估计,2016年全球27.5%的人口缺乏身体活动。在英国,2018年,25%的16岁以上的人被认为身体活动不活跃。
有证据表明,PA是痴呆的重要可改变因素,较高水平的PA被认为可能对该疾病具有保护作用。事实上,2020年发布的最新痴呆症专家报告确定了与痴呆症相关的12个主要危险因素,这些因素共同归因于40%的痴呆症病例,其中PA就是一个关键因素。

然而,迄今为止,有助于理解PA与痴呆风险关联的证据主要来自主观和自我报告数据的研究。这些数据容易出现回忆偏差,特别是在区分活动水平和强度方面,后者可能掩盖了与痴呆症关联的真实性质和程度。此外,没有证据表明设备测量的PA与痴呆结果之间的剂量 - 反应关联,这将有助于为预防痴呆的建议提供信息。本研究旨在使用英国生物银行研究探索设备测量的PA与痴呆发病率和常见亚型(AD和血管性痴呆)风险的关联,这是迄今为止最大的设备测量PA前瞻性队列。
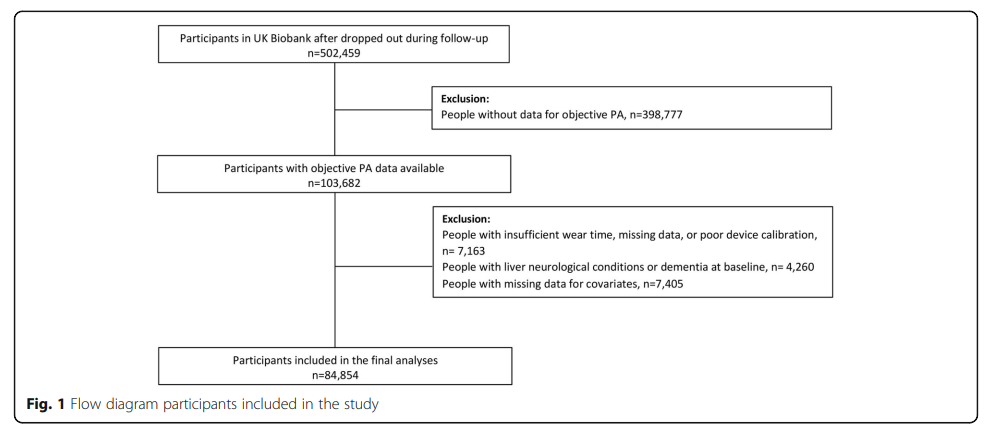
排除了在基线时加速度计测量,协变量和痴呆或神经系统疾病数据缺失的人后,84,854人纳入了这项前瞻性研究(图1)。
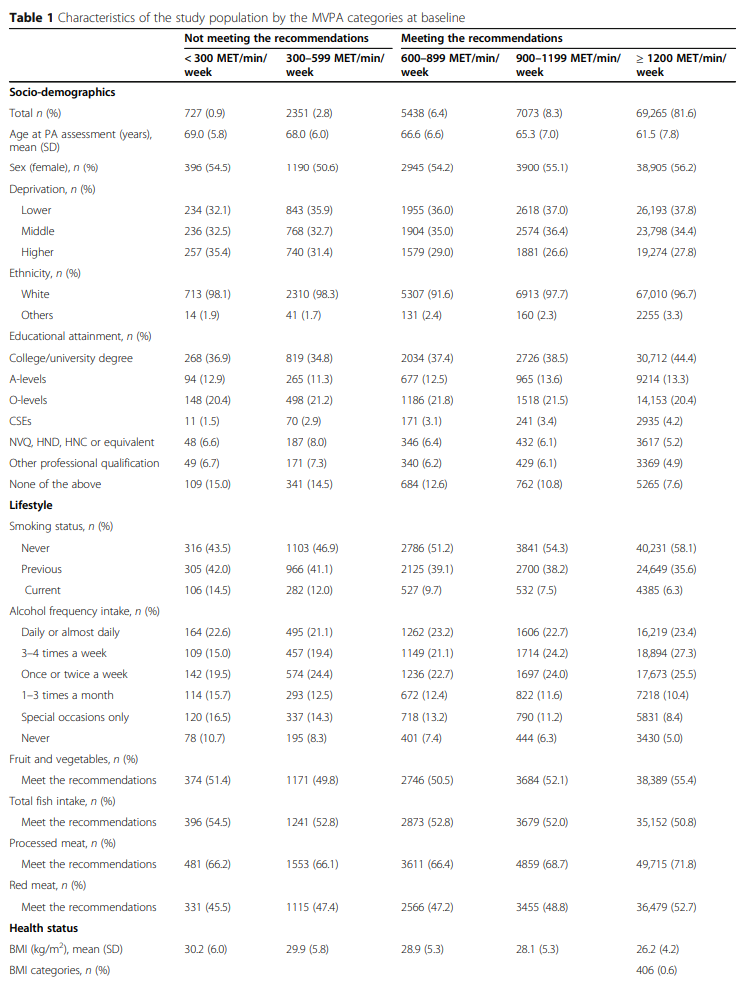
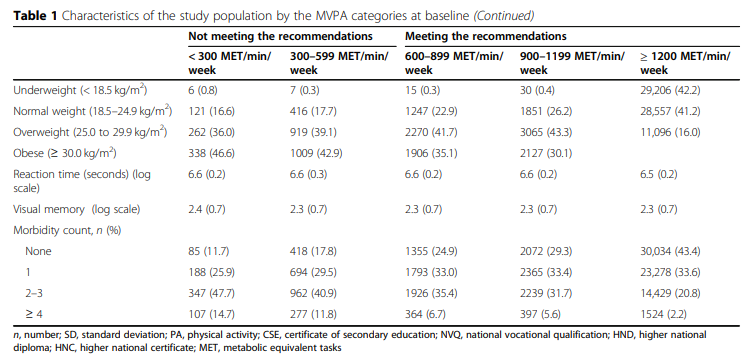
按 MVPA 类别划分的队列特征如表1所示。总的来说,比起那些活动量较低(<300 MET/min/周MVPA)的个体,MVPA水平较高的个体较年轻,更少可能有贫困社会经济状况,超重或肥胖,目前吸烟,或有一种以上的疾病。她们也更有可能是女性,受过高等教育,每周饮酒3-4次,并且遵循水果和蔬菜、加工肉类和红肉摄入的推荐建议(表1)。
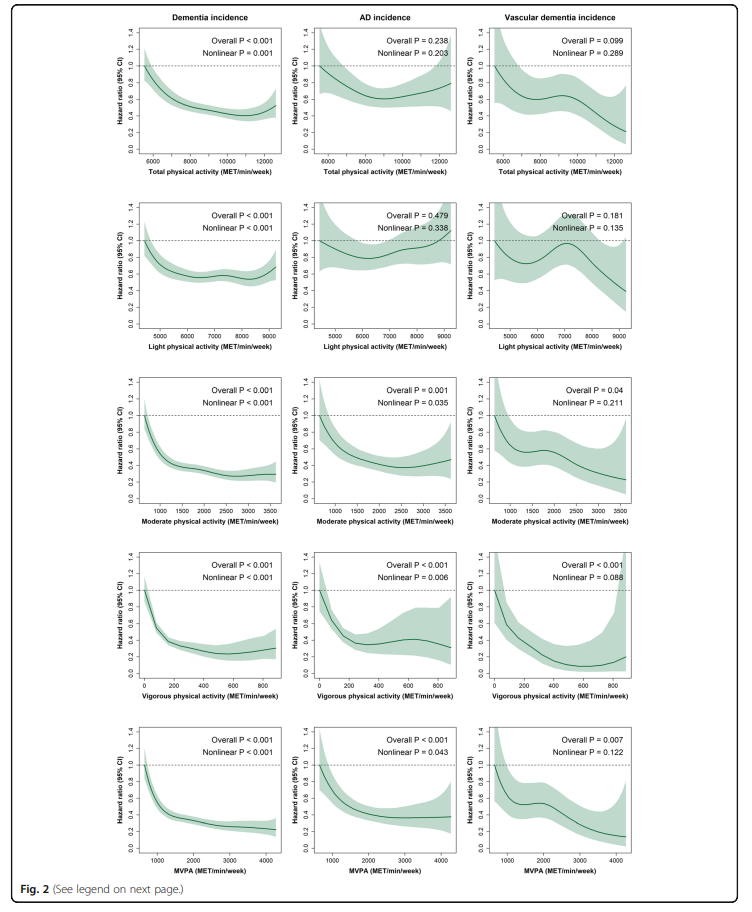
中位随访时间为6.3年(四分位间范围为5.8-6.8年)。期间678名(0.8%)参与者被诊断出患有痴呆症。图2显示 PA 模式与痴呆发生率(包括 AD 和血管性痴呆)之间的剂量-反应关联。与较少运动的人相比,保持7000 - 8000 MET/min/周的总PA的痴呆发病率降低约50%;即使在总PA保持10,000到11,000 MET/min/周的患者中,痴呆的风险降低了60%,但在这一点上没有观察到进一步的好处。在轻PA方面,那些轻PA的上限相当于~ 6000 MET/min/周的人,痴呆症发病率降低了40%,并且超过此点的估计值相似。与最不活跃的相比,对于中度PA和MVPA,1000 MET / min /周与痴呆发生率降低约60%相关。在那些每周进行2500 MET / min /周的中度PA或MVPA的人中,痴呆症的风险降低了约70%,除此之外没有观察到进一步的益处)。
对于剧烈的PA,在200 - 400 MET/min/周的个体中,痴呆发病率的风险降低了60 - 70%。在400 MET/min/周后,该关联略有持平。此外,有明确的证据表明所有PA模式和全因痴呆均存在非线性关联(P非线性<0.001)。除轻度PA外,在AD和血管性痴呆方面观察到与痴呆报告的风险估计相似,但置信区间更宽。
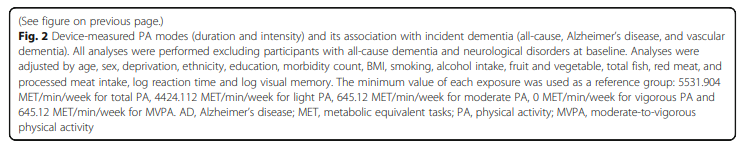
就MVPA的类别而言,当达到更高水平的MVPA时,总体痴呆(包括AD和血管性痴呆)的风险呈低趋势(图3)。与MVPA最低类别(<300 MET / min /周)的个体相比,在300至599 MET / min /周之间的人的痴呆风险降低了48%,而那些达到指南并达到600 - 899,900 - 1199或≥1200 MET/min/周的患者痴呆风险分别降低69%,76%和84%(图3)。这些关联在幅度上略有减弱,但在基线时排除CVD,高血压和糖尿病患者(敏感性分析1)以及排除基线时有疾病受试者后(敏感性分析2),仍然具有显著性(表S1)。就痴呆的亚型而言,我们发现那些达到至少600 MET/ min/周的患者发生AD的风险较低(图3)。这些关联在敏感性分析 1 中仍然显著,但在敏感性分析 2 中减弱,其中只有趋势与AD发病率之间的关联仍然显著(HR趋势0.68 [95% CI 0.50 , 0.93])(表S1)。对于血管性痴呆,仅在MET值超过900 /min/周的个体中观察到较低的风险(图3);然而,在排除基线时患有主要疾病和任何发病率的人后,关联减弱,或者没有足够的能力对这些结局进行敏感性分析。
此外,当MVPA和痴呆症类别之间的累积粗危害率由随访时间和年龄确定时,我们发现,与执行≥300 MET / min /周MVPA的个体相比,那些没有执行的人梯度曲线更陡峭。据随访和年龄计算的AD和血管性痴呆的粗危险率见图S3至S6。

最后,基于RAPs分析(表2),最不活跃参与者(MVPA为300 MET / min / 周)估计的痴呆发生率,与MVPA水平较高的患者(300 - 599;600 - 899;900 - 1199;≥1200 MET/min/周),年龄分别增加4.4岁、7.9岁、9.6岁和12.3岁时的发生率相当。除了一些例外,AD和血管性痴呆也有类似的趋势(但CI范围更广,表2)。

综上,本研究结果表明,设备测量的PA与痴呆症风险之间存在剂量反应关系,独立于社会人口学、生活方式和与健康相关的混杂因素。当分析局限于没有发病的个人时,观察到类似的结果,特别是对于全因痴呆。当研究MVPA类别和痴呆风险之间的关系时,观察到MVPA水平越高,痴呆风险越低。这种较低的风险甚至能在完成300至599 MET / min /周的个体中观察到 -——即虽然低于每周每分钟600 MET以上的身体活动建议,他们患痴呆症的风险降低了48%。后者支持世界卫生组织的说法,即"每一步都很重要",并且应鼓励PA作为痴呆症风险的保护因素。在执行超过1200 MET / min /周的个体中发现风险最低,与那些执行<300 MET / min /周的患者相比,事件性痴呆风险降低84%(95%CI 0.12至0.21)。此外,如果我们考虑到达到300 MET/min/周以上的MVPA可能会将痴呆症延迟4.4至12年(对于那些表现在300至≥1200 MET / min /周的人),在整个生命周期中需要公共策略,尤其是那些风险较高的个体。
总的来说,在不考虑PA类型的情况下,具有较高PA测量值的个体比那些不那么活跃的个体发生痴呆的风险更低。考虑到以前的大多数研究都使用自我报告的数据报告了这种关联,本研究结果强调了PA和痴呆发病之间的强反向剂量-反应关联。对于痴呆症,我们还证明所有PA强度和持续时间都是重要的,因为它们都与全因痴呆症的风险较低有关。
最后,考虑到经常运动的人可能比那些不经常运动的人晚12年发生痴呆,应该在整个生命周期中优先考虑制定公共卫生政策来提高PA水平,尤其是对那些患痴呆风险较高的人。
原文来源:
Petermann-Rocha et al.Dose-response association between device-measured physical activity and incident dementia: a prospective study from UK Biobank.BMC Medicine (2021) 19:305
https://doi.org/10.1186/s12916-021-02172-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














撸铁
115
#痴呆风险#
68
合理运动是个宝
139
签到
130
好的!
130
好文章,谢谢分享。
144
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
70