心脏骤停是指心脏突然停止射血,造成循环停止而产生的一系列症状体征,包括意识丧失、晕厥、 大动脉搏动消失等。心脏骤停是猝死的重要原因。心脏骤停根据其机制可分为4种情况:心室颤动、无脉搏室性心动过速、心脏静止和电机械分离。 前两种被称为“可复律”心脏骤停。
一,治疗原则
心脏骤停一旦发生,及时有效的心肺复苏至关 重要。心脏骤停发生后 4 min 内为抢救的最佳时机,这一时间内给患者实施有效的心肺复苏或识别心律失常,尽早除颤,患者的生命极有可能被挽回 。心脏骤停的药物主要用在第二次除颤不成 功后,在除颤同时给予抗休克药物、抗心律失常药 物及酸碱平衡调节药物。若监测显示为不可除颤 心律(如心脏停搏或电机械分离),建议持续心肺复苏,并尽早静脉推注肾上腺素 ;若为可除颤心律, 经推注1~2次肾上腺素并除颤后仍无效时,可经静 脉给予胺碘酮;若患者存在明显代谢性酸中毒 或高钾血症,可静脉给予碳酸氢钠。
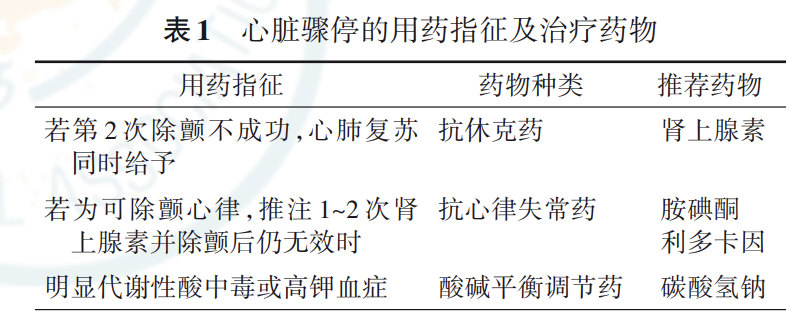
二,治疗药物
(一)肾上腺素
1,药品分类:抗休克药。
2,用药目的:用于各种原因引起的心脏骤停进 行心肺复苏抢救。
3,禁忌证:作为心脏骤停行心肺复苏抢救用药 时无禁忌证。
4,不良反应:心悸、头痛、血压升高、震颤、无 力、眩晕、呕吐、四肢发凉;有时可有心律失常;用药 局部可有水肿、充血、炎症。
5,药物相互作用:α受体阻滞剂以及各种血管 扩张药可对抗肾上腺素的加压作用;与全麻药、洋 地黄、三环类抗抑郁药合用,可致心律失常;与麦角 制剂合用,可致严重高血压和组织缺血;与利血平、 胍乙啶合用,可致高血压和心动过速;与 β 受体阻 滞剂合用,两者的 β 受体效应互相抵消,可出现血 压异常升高、心动过缓和支气管收缩;与硝酸酯类 药物合用,本品的升压作用被抵消,硝酸酯类药物 的抗心绞痛作用减弱。
(二)胺碘酮
1,药品分类:Ⅲ类抗心律失常药。
2,用药目的:用于体外电除颤无效的室性心动 过速、心室颤动相关心脏停搏的心肺复苏。 3,禁忌证:用于体外电除颤无效的室性心动过 速、心室颤动相关心脏停搏的心肺复苏时无禁 忌证。
4,不良反应及处理:可能出现角膜微沉积、甲 状腺激素水平异常、睡眠障碍、头痛、梦魇、感觉、运 动或混合性周围神经病变、血清转氨酶增高、凝血 异常、胃肠道异常(恶心、呕吐、厌食和便秘)、乏力、 震颤、不自主运动、步态异常/共济失调或其他锥体 外系症状,停止胺碘酮治疗后通常完全可逆;光过 敏反应,应避免暴露于阳光(以及紫外光)下;弥漫 性间质性或肺泡性肺病和闭塞性细支气管炎伴机 化性肺炎。
5,药物相互作用:胺碘酮可增加华法林的抗凝作用;可增高奎尼丁、普鲁卡因胺、氟卡尼及苯妥英 钠的浓度;与Ⅰa类抗心律失常药合用可加重QT间 期延长;与β受体阻滞剂或钙拮抗剂合用可加重窦 性心动过缓、窦性停搏及房室传导阻滞;可增加血 清地高辛浓度;与排钾利尿剂合用,可增加低血钾 所致的心律失常。
(三)利多卡因
1,药品分类:Ⅰ类抗心律失常药。
2,用药目的:用于体外电除颤无效的室性心动 过速、心室颤动相关心脏停搏的心肺复苏。 3,禁忌证:禁用于严重心脏传导阻滞,包括二 或三度房室传导阻滞,双束支传导阻滞;严重窦房 结功能障碍;对利多卡因过敏者。
4,不良反应及处理:利多卡因可作用于中枢神 经系统,引起嗜睡、感觉异常、肌肉震颤、惊厥、昏迷 及呼吸抑制等不良反应,还可引起低血压及心动过 缓;血药浓度过高,可引起心房传导速度减慢、房室 传导阻滞以及抑制心肌收缩力和心输出量下降。 停药后上述不良反应可消失。
5,药物相互作用:与西咪替丁、β 受体阻滞剂 如普萘洛尔、美托洛尔、纳多洛尔合用,利多卡因经 肝脏代谢受抑制,血浓度增加,可发生心脏和神经 系统不良反应,应调整利多卡因剂量,并应进行心 电监护及监测利多卡因血药浓度;巴比妥类药物可 促进利多卡因代谢,两药合用可引起心动过缓,窦 性停搏;与普鲁卡因胺合用,可产生一过性谵妄及 幻觉,但不影响利多卡因血药浓度;异丙基肾上腺 素因增加肝血流量,可使利多卡因的总清除率升 高;去甲肾上腺素因减少肝血流量,可使利多卡因 总清除率下降。
(四)碳酸氢钠
1,药品分类:酸碱平衡调节药。
2,用药目的:用于治疗心肺复苏后严重的代谢 性酸中毒。
3,禁忌证:禁用于代谢性或呼吸性碱中毒;因 呕吐或持续胃肠负压吸引导致大量氯丢失而极有 可能发生代谢性碱中毒;低钙血症时,因本品引起 碱中毒可加重低钙血症表现;禁用于吞食强酸中毒 时的洗胃,因本品与强酸反应产生大量二氧化碳, 导致急性胃扩张甚至胃破裂。
4,不良反应及处理:大量注射时可出现心律失 常、肌肉痉挛、疼痛、异常疲倦虚弱等,需及时补钾; 剂量偏大或存在肾功能不全时,可出现水肿、精神 症状、肌肉疼痛或抽搐、呼吸减慢、口内异味、异常 疲倦虚弱等。
5,药物相互作用:合用肾上腺皮质激素、促肾 上腺皮质激素、雄激素时,易发生高钠血症和水肿; 与苯丙胺、奎尼丁、麻黄碱合用,应减少后者的剂 量;与抗凝药(如华法林)、M 胆碱酯酶药、西咪替 丁、雷尼替丁等合用时,后者吸收减少;与含钙药物 及乳制品合用,可致乳‐碱综合征;与排钾利尿药合 用,增加发生低氯性碱中毒的危险性;可增加水杨 酸制剂、锂制剂的排泄。
原始出处
中华医学会.心脏骤停基层合理用药指南.中华全科医师杂志 2021 年3 月第 20 卷第 3 期 Chin J Gen Pract, March 2021, Vol. 20, No. 3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












好好学习
90
学习了
124
好文章
102
学习了
89
#合理用药#
88