JNCCN:神经内分泌肿瘤(NETs)患者肿瘤特异性死亡的风险
2021-06-06 yd2015 MedSci原创
神经内分泌肿瘤(NETs)整体人群患者的肿瘤特异性死亡风险较非肿瘤相关死亡高。不同部位的肿瘤患者存在较强异质性。对于非转移性胃肠NETs患者,非肿瘤相关死亡率高于肿瘤特异性死亡。
神经内分泌肿瘤(NETs)正在逐渐被人们所熟悉。NETs是一类特异性很强的肿瘤,伴有多变的生物学行为、临床和预后特征。但是,神经内分泌肿瘤(NETs)造成的肿瘤负担、肿瘤特异性死亡以及预后因素等信息还不是很明确。因此,来自加拿大的研究团队开展了一项回顾性研究,评估神经内分泌肿瘤(NETs)患者肿瘤特异性死亡和非肿瘤性死亡的累积发生率。相关研究成果发表在Journal of the National Comprehensive Cancer Network(JNCCN)杂志上。

该研究是一项基于人群的回顾性队列研究,纳入加拿大2001年至2015年登记的NETs患者。评估原发性NETs和不同转移状态下患者的肿瘤特异性死亡和非肿瘤性死亡的累积发生率。研究共纳入8607例患者,中位随访42个月(范围:17-82个月)。最常见的原发肿瘤部位为支气管肺(22.8%),其次为小肠(19.3%)和直肠(14.4%)。42.2%患者伴有有转移,包括32.0%患者伴有同时性转移。
NETs整体人群患者的5年肿瘤特异性死亡风险较非肿瘤相关死亡高,死亡率分别为7.3%(95% CI, 26.3%–28.4%) 和 5.6% (95% CI, 5.1%–6.1%)。而10年的肿瘤特异性死亡率和非肿瘤相关死亡率分别为34.5% (95% CI, 33.2%–35.8%)和10.3% (95% CI,9.4%–11.3%)。伴有转移的NETs患者,包括同时性和异时性转移,肿瘤特异性死亡率高于非肿瘤相关死亡。而不伴有转移的NETs患者,两组死亡方式的比例相近。
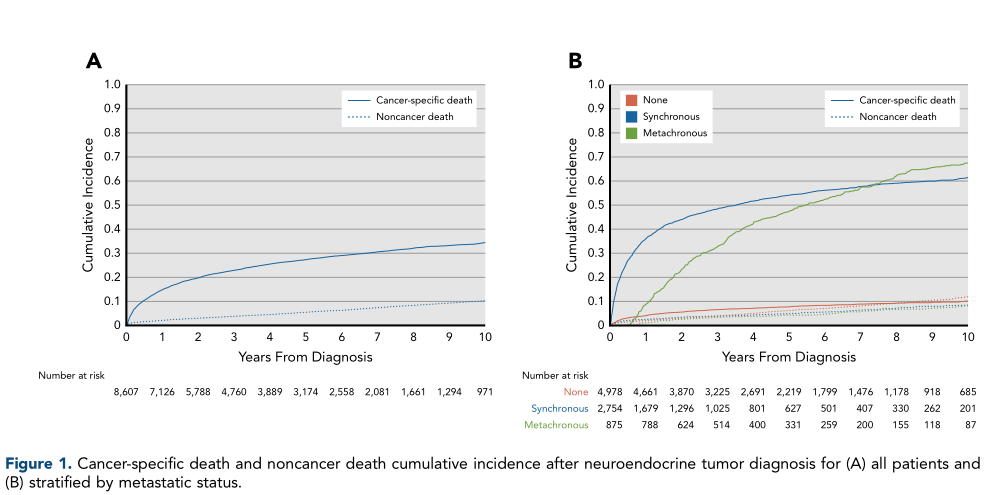
NETs整体人群肿瘤和非肿瘤死亡率
原发性支气管肺NTEs患者的肿瘤特异性性死亡率最高,5年和10年肿瘤特异性死亡率分别为36.4%(95% CI, 34.2%–38.7%)和42.7% (95% CI,0.1%–45.3%)。转移性和非转移性支气管肺NTEs患者的肿瘤特异性死亡率均高于非肿瘤相关死亡。
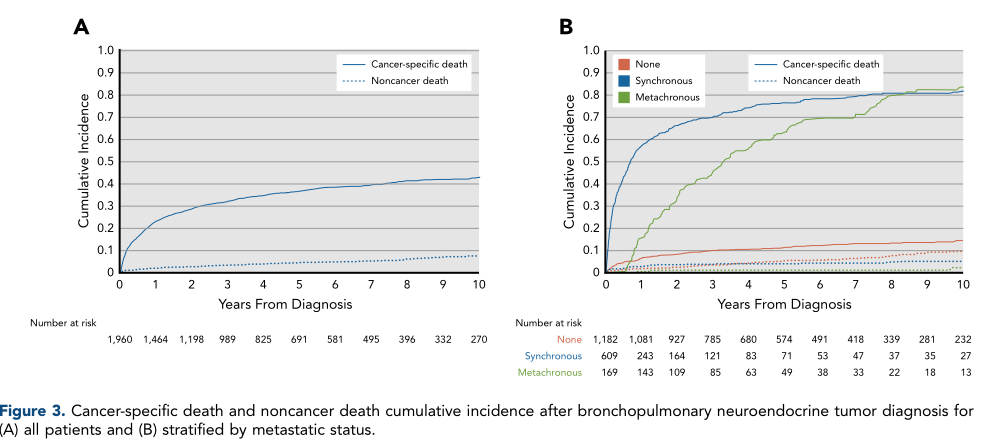
原发性支气管肺NTEs患者肿瘤特异性和非肿瘤死亡
原发性胰腺NETs患者5年和10年肿瘤特异性死亡率分别为34.8% [95% CI, 31.5%–38.2%] 和48.4% [95% CI, 43.5%–53.0%]。转移性和非转移性胰腺NTEs患者的肿瘤特异性死亡率均高于非肿瘤相关死亡。
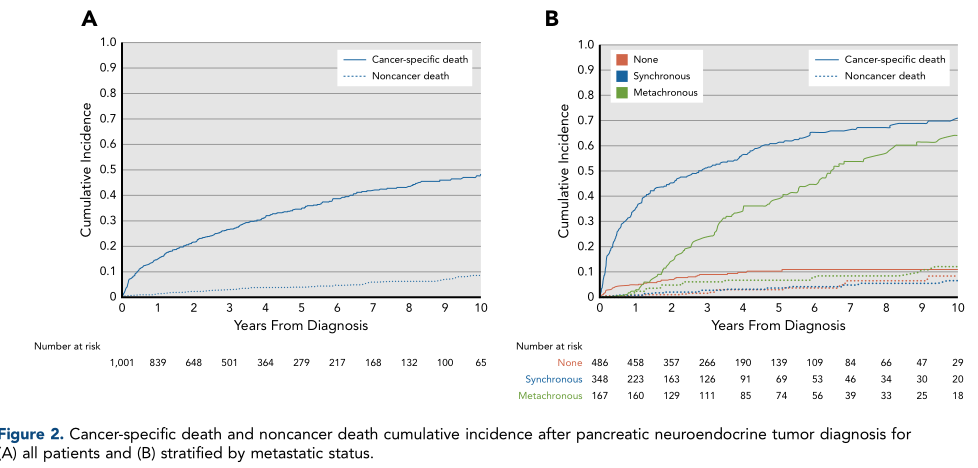
原发性胰腺NTEs患者肿瘤特异性和非肿瘤死亡
原发性结肠NETs 患者5年和10年肿瘤特异性死亡率分别为21.4%[95%CI, 18.9%–24.0%]和26.6% [95% CI, 23.4%–29.9%]。对于非转移性NTEs患者,非肿瘤相关死亡率高于肿瘤特异性死亡率。比如非转移性胃NETs患者的5年和10年非肿瘤相关死亡率分别为10.4% (95%CI,7.1%–14.4%)和18.9% (95% CI, 13.4%–25.2%);而肿瘤特异性死亡率分别为 5.8% (95%CI,3.5%–8.9%)和9.0% (95%CI, 5.1%–14.3%)。非转移性小肠NETs患者的5年和10年非肿瘤相关死亡率分别为13.0% (95% CI,10.2%–16.0%)和22.4% (95% CI, 17.7%–27.4%);而肿瘤特异性死亡率分别为 4.7% (95% CI,3.1%–6.7%) 和8.6% (95% CI, 5.7%–12.3%)。非转移性结肠NETs患者的5年和10年非肿瘤相关死亡率分别为6.4% (95% CI, 4.5%–8.8%)和11.4%(95% CI, 7.9%–15.6%);而肿瘤特异性死亡率分别为4.1% (95% CI, 2.7%–5.9%)和5.9% (95% CI, 3.8%–8.6%)。非转移性直肠NETs患者的5年和10年非肿瘤相关死亡率分别为2.7% (95% CI, 1.8%–3.9%)和6.6% (95% CI,4.7%–9.0%);而肿瘤特异性死亡率分别为7.4% (95% CI, 5.9%–8.9%) 和 9.3% (95% CI,7.4%–11.4%)。
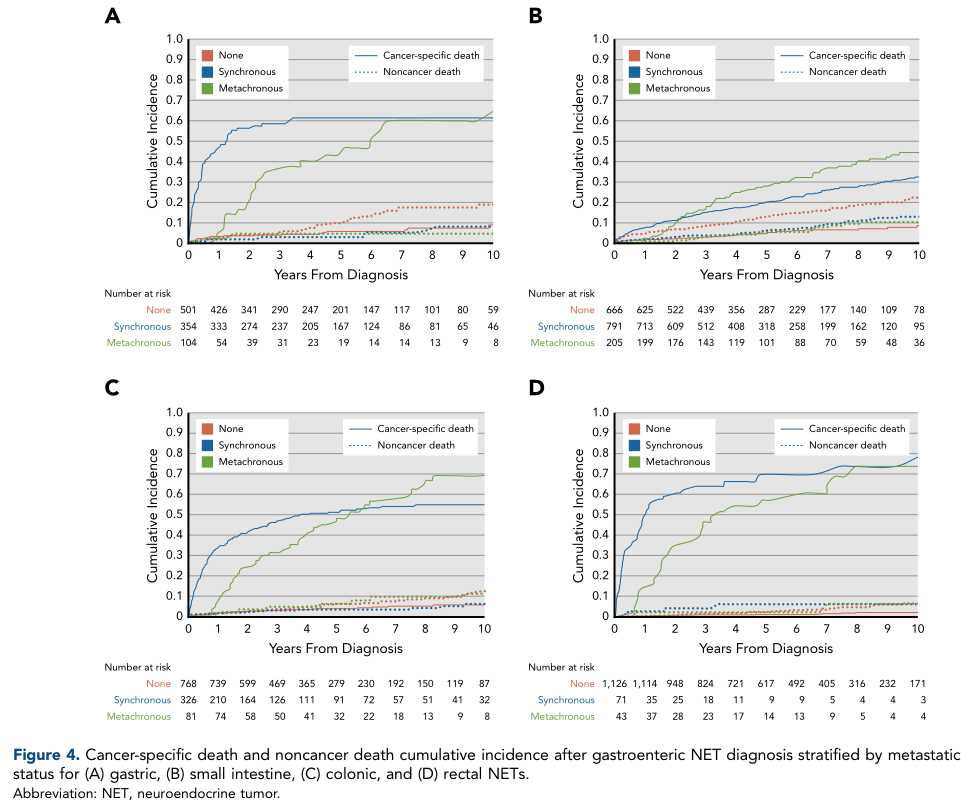
胃肠NTEs患者肿瘤特异性和非肿瘤死亡
多因素分析发现,老年、物质匮乏和转移跟高肿瘤特异性死亡风险有关,而女性和伴随疾病跟较低肿瘤特异性死亡风险有关。
综上,神经内分泌肿瘤(NETs)整体人群患者的肿瘤特异性死亡风险较非肿瘤相关死亡高。不同部位的肿瘤患者存在较强异质性。对于非转移性胃肠NETs患者,非肿瘤相关死亡率高于肿瘤特异性死亡。
原始出处:
Julie Hallet, Calvin Law, Simron Singh, et al. Risk of Cancer-Specific Death for Patients Diagnosed With Neuroendocrine Tumors: A Population-Based Analysis. J Natl Compr Canc Netw. 2021 Jun 4;1-10. doi: 10.6004/jnccn.2020.7666. Online ahead of print.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#内分泌肿瘤#
67
#神经内分泌#
67
#分泌#
55
#NET#
76
#特异性#
66
#NCCN#
52
#NETs#
76