Cancer Cell:S1PR1-STAT3激活促进骨髓样细胞的促肿瘤转移作用
2012-05-24 Victor 生物谷
近来研究表明,骨髓样细胞可使远处器官易于接受扩散肿瘤细胞的集落形成。然而,其具体机制一直不明。5月14日Cancer Cell报道了Hua Yu研究组的论文"S1PR1-STAT3 Signaling Is Crucial for Myeloid Cell Colonization at Future Metastatic Sites"揭示了其分子机制。 研究者发现,在肿瘤细胞中

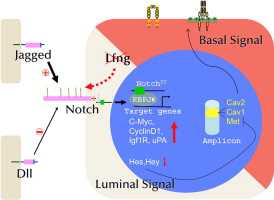
近来研究表明,骨髓样细胞可使远处器官易于接受扩散肿瘤细胞的集落形成。然而,其具体机制一直不明。5月14日Cancer Cell报道了Hua Yu研究组的论文"S1PR1-STAT3 Signaling Is Crucial for Myeloid Cell Colonization at Future Metastatic Sites"揭示了其分子机制。
研究者发现,在肿瘤细胞中神经鞘氨醇-1-磷酸化受体-1(S1PR1)-STAT3信号通路上调可激活肿瘤转移靶部位细胞的S1PR1-STAT3水平,在机体远处组织造成易于接受转移肿瘤的微环境。抑制S1PR1或者STAT3在骨髓样细胞中的功能可破坏已存在的易转移微环境。
S1PR1-STAT3信号通路的激活使骨髓样细胞能穿过血管,在远处器官形成利于肿瘤转移的微环境并且介导其自身及其他基质细胞持续的存活和增殖。对肿瘤患者不含肿瘤细胞的淋巴结的分析发现,与正常人的淋巴结细胞相比,肿瘤患者的标本呈现更高的骨髓样细胞浸润,STAT3的高水平活化以及细胞存活信号的增强。(生物谷Bioon.com)

doi: 10.1016/j.ccr.2012.03.039
PMC:
PMID:
S1PR1-STAT3 Signaling Is Crucial for Myeloid Cell Colonization at Future Metastatic Sites
Jiehui Deng, Yong Liu, Heehyoung Lee, Andreas Herrmann, Wang Zhang, Chunyan Zhang, Shudan Shen, Saul J. Priceman, Maciej Kujawski, Sumanta K. Pal, Andrew Raubitschek, Dave S.B. Hoon, Stephen Forman, Robert A. Figlin, Jie Liu, Richard Jove, Hua Yu
Recent studies underscore the importance of myeloid cells in rendering distant organs hospitable for disseminating tumor cells to colonize. However, what enables myeloid cells to have an apparently superior capacity to colonize distant organs is unclear. Here, we show that S1PR1-STAT3 upregulation in tumor cells induces factors that activate S1PR1-STAT3 in various cells in premetastatic sites, leading to premetastatic niche formation. Targeting either S1PR1 or STAT3 in myeloid cells disrupts existing premetastatic niches. S1PR1-STAT3 pathway enables myeloid cells to intravasate, prime the distant organ microenvironment and mediate sustained proliferation and survival of their own and other stromal cells at future metastatic sites. Analyzing tumor-free lymph nodes from cancer patients shows elevated myeloid infiltrates, STAT3 activity, and increased survival signal.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
111
#Cell#
114
#STAT3激活#
124
#cancer cell#
150
#肿瘤转移#
133
#STAT3#
126