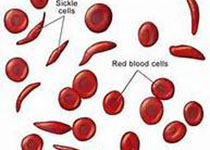
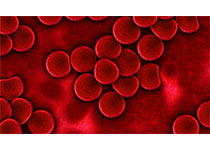
PNAS:红细胞成熟机制新发现——有望治疗特定类型贫血
2017-09-06 佚名 medicalxpress
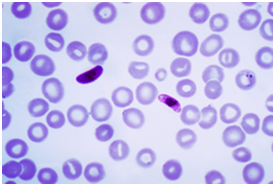
一个多世纪以来,医生有传言指出,甲状腺功能低下的患者常常由于碘缺乏引起贫血。但是甲状腺激素和红细胞之间的联系仍然不是很清楚。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PNAS#
75
#新发现#
67
#特定类型#
83
#红细胞#
82