颅骨胆脂瘤术后并发硬膜下血肿1例
2020-07-24 惠卫宁 邵国平 褚荣涛 临床神经外科杂志
胆脂瘤即表皮样囊肿,多见于桥小脑角区,较少起源于颅骨;其术后并发硬膜下血肿者鲜有报道。常熟市第二人民医院近期收治1例右额颞部颅骨胆脂瘤患者。行手术切除肿瘤后,术中硬脑膜完整,并发硬膜下血肿;经颅骨钻孔
胆脂瘤即表皮样囊肿,多见于桥小脑角区,较少起源于颅骨;其术后并发硬膜下血肿者鲜有报道。常熟市第二人民医院近期收治1例右额颞部颅骨胆脂瘤患者。行手术切除肿瘤后,术中硬脑膜完整,并发硬膜下血肿;经颅骨钻孔血肿清除术治疗恢复正常。现对患者的临床资料进行总结分析,并复习相关文献;以探讨颅骨胆脂瘤术后并发硬膜下血肿的临床特点及可能的发病机制。
1.临床资料
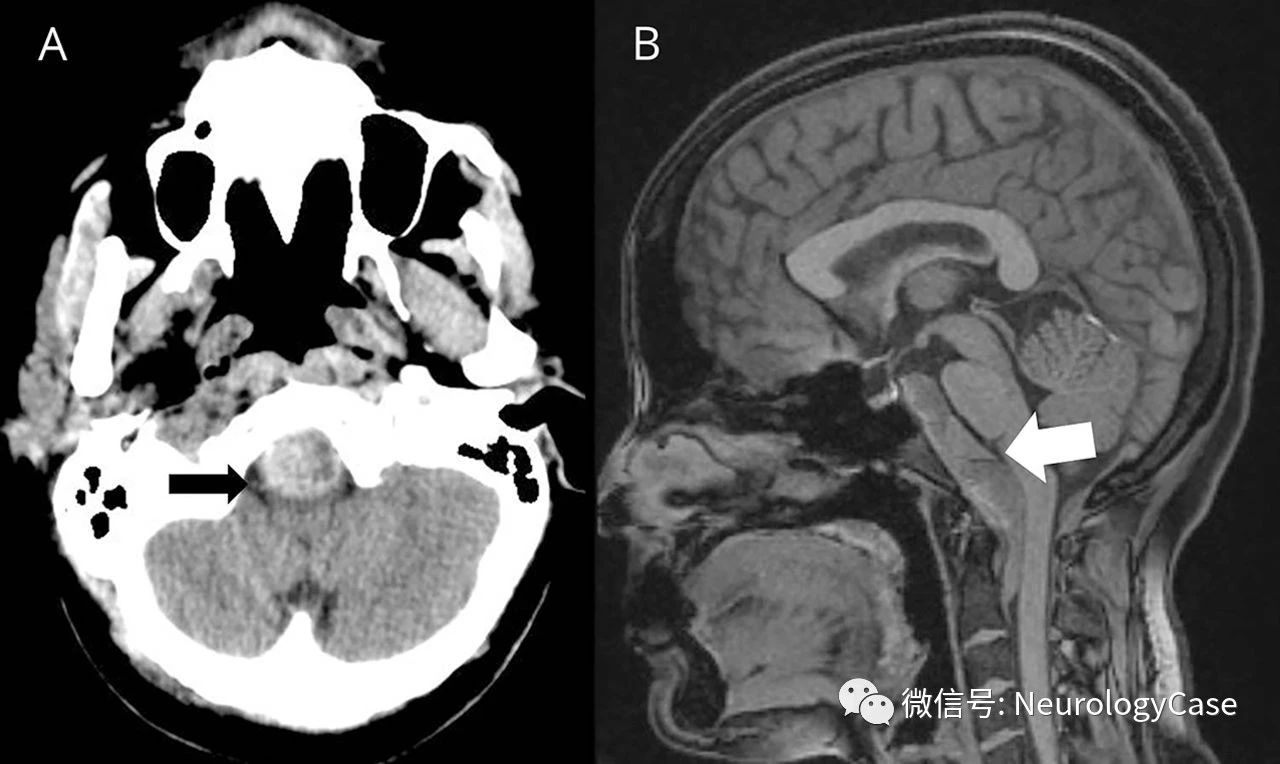
患者,男,55岁。因“右侧耳鸣2个月”于2017年12月入院。患者自入院前两个月起,无明显诱因出现右侧蝉鸣样耳鸣。查体:头颅外形正常,神经系统检查未见异常。头颅CT检查:右侧额颞部低密度占位(图1A)。头颅MRI检查示,右侧额颞部占位,为骨源性,T2WI为高信号,T1WI为低信号,混杂条索样高信号,DWI弥散受限;增强扫描,病变周边环形强化,内部无强化;见图1B、C、D。术前诊断:右侧额颞部骨肿瘤。行开颅肿瘤切除术。

图1 患者术前的影像学检查。A:头颅CT;B:头颅MRIT2WI;C:MRIT1WI;D:MRI增强扫描
在全麻下,右侧额颞翼点入路切口、骨瓣。术中见右侧额颞部颅骨外板变薄,内板侵蚀破坏(图2A);肿瘤组织为白色粘稠豆腐渣样,有薄层囊壁,大部分与硬脑膜界限清楚,少部分与硬脑膜粘连;除囊壁外,肿瘤组织无血供(图2B)。将肿瘤组织连同包膜全部切除,硬脑膜完整,骨瓣磨除受侵蚀部分后予以复位;硬膜外置负压引流管。术后第2d引流管无明显引流物,予以拔除。术后肿瘤组织病理检查为颅骨胆脂瘤(图3)。

图2 手术中所见。A:受侵犯的颅骨外板变薄,内板侵蚀破坏;B:肿瘤组织为白色粘稠豆腐渣样,有薄层囊壁
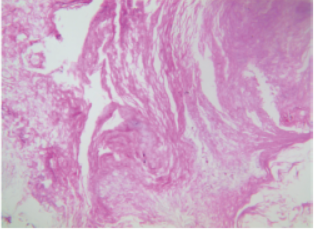
图3肿瘤组织病理学检查(HE染色,×200)
术后第3d患者出现意识障碍;复查头颅CT示,右侧额颞部硬膜下新月形等低密度影,考虑血肿(图4)。即行颅骨钻孔硬膜下血肿清除术;术中见硬膜下血肿为不凝固暗红色血液及棕黄色水样物,有假包膜形成,为灰白色胶冻样物,内层覆盖于脑表面,外层位于硬脑膜内面,触之有少量出血。血肿液培养无细菌生长。血肿清除术后患者的意识障碍逐渐恢复正常;1周后复查CT示,右侧额颞部硬膜下血肿明显减少;出院。出院后半个月,患者复查CT示血肿完全吸收,意识状态正常。

图4 肿瘤切除术后第3d头颅CT复查示右侧额颞部硬膜下血肿
2.讨论
颅骨胆脂瘤是因胚胎发育过程中外胚层的组织异位到颅骨而形成。原发颅骨胆脂瘤较少见,肿瘤多位于颞前部和额顶部,多起源于板障内。肿瘤的组织结构由薄层的囊壁和囊内容物两部分构成,囊壁由复层鳞状上皮和薄层结缔组织组成,内容物为角化脱落上皮、干酪样物质、胆固醇结晶。
在早期颅骨破坏之前,患者一般无临床症状;肿瘤如向内生长可出现脑组织压迫症状、癫痫发作等;向外生长,可以出现颅骨肿物、缺损、感染窦道等。CT检查示肿瘤为低密度影,甚至可低于脑脊液;颅骨内外板膨胀变薄,邻近颅骨呈喇叭样,边界清楚,边缘可有硬化;肿瘤无增强。
MRI检查,肿瘤在T2WI为显著高信号;T1WI信号多变,主要与内容物成分有关;胆固醇结晶在CT上呈均匀低密度,在T1WI为均匀低信号;角化物和高蛋白成分在CT上为稍高、等、稍低混杂密度,在T1WI为高信号影。颅骨胆脂瘤根据囊内成分特点及颅骨特征性改变诊断不难,但要与嗜酸性肉芽肿、颅骨骨巨细胞瘤、皮样囊肿、血管瘤及转移瘤等鉴别。嗜酸性肉芽肿常多发,大小不等的颅骨地图状缺损,缺损区有“纽扣状”死骨征象。
颅骨巨细胞瘤好发于颞骨及蝶骨,偶见于顶骨及额骨,CT表现多为膨胀性生长;肿瘤多向周围组织侵犯,多并发软组织肿块,并侵及周围肌肉。皮样囊肿囊内含有凡士林样脂性物质,CT上密度更低,MRI上呈短T1,壁厚可出现钙化。血管瘤骨质破坏区,MRI增强扫描有明显强化,并可见粗大颅内血管进入瘤区。颅骨溶骨性转移瘤,结合病史诊断不难。本例患者虽然在发病时间上不符合慢性硬膜下血肿的诊断标准,但是根据手术前后的CT表现、术中所见,术后恢复情况,均符合慢性硬膜下血肿的病理改变及转归。
慢性硬膜下血肿绝大多数与轻微头部外伤有关,非损伤性慢性硬膜下血肿比较少见,可能与脑血管病变、炎症产生多种炎症因子有关,确切机制尚不完全清楚。在病理学表现上,慢性硬膜下血肿有内外两层壁,内层为胶原物质,无血管,外层也是胶原物质,内含壁不完整的毛细血管网,容易有血细胞漏出;毛细血管内皮细胞间隙可见变形红细胞;血肿液的蛋白组学分析显示,血肿液与血液具有非常相似的蛋白组学。
目前认为慢性硬膜下血肿是一种炎症性疾病;其中炎性因子、趋化因子和血管生成因子等多种炎症因子的共同作用,可能是慢性硬膜下血肿形成的关键因素。研究发现,血肿液中的炎性因子白介素(IL-6、IL-8、IL-10)水平明显高于外周血;并且血肿腔外膜血管内皮生长因子(vascular endothelial growth factor,VEGF)的表达也显著升高;这些细胞因子水平与血肿复发关系密切。还有研究发现,血肿液中血管生成相关因子胎盘生长因子(PIGF)、VEGF、成纤维细胞生长因子(bFGF)、基质金属蛋白酶(MMP)表达水平显著升高,血肿外膜中血管生成素(angiogenin,Ang)1、Ang-2mRNA升高,提示新血管生成增多。
血肿液中调节炎症反应及血管生成的趋化因子CCL2、CXCL8、CXCL9及CXCL10表达也升高。一项多中心双盲对照试验结果显示,抗炎药物地塞米松可以有效减少慢性硬膜下血肿术后复发。此外,血肿液凝血功能障碍,如血肿液及外膜中组织型纤溶酶原激活物、纤维蛋白降解产物及血栓调节蛋白水平明显升高,而凝血因子Ⅱ、Ⅴ、Ⅷ水平下降。
本例患者根据术前CT及MRI检查及结合术后病理检查结果,颅骨胆脂瘤的诊断明确。术中硬脑膜完整,术后短时间内出现骨瓣下硬膜下血肿;血肿清除术中所见与慢性硬膜下血肿符合;其确切机制有待进一步病例积累分析。有研究发现,胆脂瘤肿瘤细胞可以表达、产生多种炎症相关物质,参与炎症反应。
本例患者的发病机制可能为,术后硬膜外肿瘤包膜破裂、内容物外泄,外泄物质中有致炎症因子,与硬脑膜接触,刺激硬膜发生无菌性炎症,出现硬膜下无菌性炎症、渗出,并形成炎性假性包膜;假包膜外壁新生毛细血管内红细胞漏出,形成硬膜下血肿。所以,颅骨胆脂瘤切除术中应尽量保持肿瘤包膜完整,实施包膜外完整切除,并减少包膜残留;术毕应充分冲洗术野,减少肿瘤中脂类物质、炎症因子的残留。
另外,术后常规动态检查头颅CT,警惕术后并发硬膜下血肿。一旦发生硬膜下血肿,必要时应及时行颅骨钻孔血肿清除手术;再次手术尽量避开原来的切口,以降低颅内感染风险。
原始出处:
惠卫宁,邵国平,褚荣涛,黄炜,李向东,惠国祯.颅骨胆脂瘤术后并发硬膜下血肿1例报告并文献复习[J].临床神经外科杂志,2019,16(03):259-261.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#硬膜下#
75
#并发#
54
#血肿#
84
#硬膜下血肿#
85
#胆脂瘤#
62