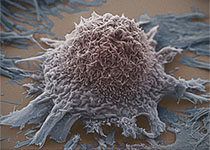
2017 CSCO:蔡三军教授:非手术治疗可能是针对进展期直肠癌更有价值的治疗
2017-09-30 MedSci MedSci原创
2017年9月26日-30日,备受业内瞩目的“第20届全国临床肿瘤大会暨2017年CSCO学术年会”在厦门隆重开幕。本届年会以“传承创新,携手同行”为主题,并继续秉承CSCO的根本宗旨,开展了多种形式的继续教育和学术交流活动。在此次大会上,来自复旦大学附属肿瘤医院大肠外科的中国临床肿瘤协作中心(CSCO)常委、继续教育委员会主任——蔡三军教授围绕“局部晚期直肠癌wait and see 治疗策略进
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#蔡三军#
71
#进展期#
85
学习了谢谢作者分享!
0
#手术治疗#
60
#非手术治疗#
78
学习了
0
继续学习中谢谢
87
已学习.值得分享!
95
好资料学习了!
109