ACC.21|LAAOS III:左心耳封堵预防房颤相关卒中再添新证北医三院唐熠达教授团队:
2021-05-16 “心关注”公众号 “心关注”公众号
左心耳是房颤患者血栓形成主要部位。左心耳封堵(LAAO)是否可降低房颤患者的卒中风险是业界的重要假说之一,但一直未被有力证据正证实。近期以Whitlock RP为首的心外科及房颤领域专家共同进行了LA
左心耳是房颤患者血栓形成主要部位。左心耳封堵(LAAO)是否可降低房颤患者的卒中风险是业界的重要假说之一,但一直未被有力证据正证实。近期以Whitlock RP为首的心外科及房颤领域专家共同进行了LAAOS III研究,探索了LAAO在预防房颤卒方面的作用。该研究为随机、双盲、多中心设计,证据等级高。该研究结论对临床治疗策略有重大影响,近期发表于新英格兰杂志,并在AHA2021年年会上做了“最新临床试验突破”报告,值得引起足够重视。
该研究证实房颤卒中高危患者中,在接受心脏其他手术时同期以外科方式封堵左心耳可显着降低缺血性脑卒中风险,且该获益独立于口服抗凝药之外,亦不增加心衰等不良事件风险。此外,由于长期口服抗凝药存在出血风险增加、需要剂量调整、依从性差等问题,该研究还启发人们思考是否外科LAAO是否可替代口服抗凝药。随着内科封堵器的有效性、安全性被逐渐接受,心脏外科同期LAAO的价值值得探索。
研究背景
ACC.21|LAAOS III
- 假说认为左心耳封堵(LAAO)可以预防房颤相关卒中;
- 在其他心脏手术同期行LAAO简便易行;
- 该研究旨在评价在其他心脏手术同期行LAAO是否可降低房颤患者卒中及系统性栓塞风险。
研究方法
ACC.21|LAAOS III
入组对象为拟行心脏外科手术且CHA2DS2-VASc≥2分的房颤患者。随机分为LAAO组、非LAAO组。
- 盲法:研究对象、研究团队、治疗团队接受盲法。
- 干预措施:LAAO组患者接受以下三种方式中的一种干预左心耳,即①心外膜夹闭左心耳根部;②左心耳切除后缝扎;③心外膜器械封堵。
- 首要结局:卒中或系统性栓塞。
- 首要安全结局:因心衰住院。
- 分析策略:对所有研究对象进行意向性分析。以术后30天记,进行二次界标分析(意在观察非手术急性期事件风险)。
- 随访方式:①每6个月以卒中问卷的方式随访一次;②所有研究对象按日常诊疗方式处理;③安全监察委员会负责按计划终止研究并进行中期分析。
研究结果
ACC.21|LAAOS III
本研究共入组来自27个国家、105个中心的4811名患者,平均随访3.8年。最终2379名患者接受了LAAO,对照组2391名患者,基线资料见表1。两组患者其他心脏手术方式大致相似(表2)。LAAO组患者手术时间稍长(p<0.001),其余手术相关安全事件无明显差别。30天死亡率均<5%,无显着差异(表3)。出院时两组患者抗凝率逾80%;随访至第3年时,两组患者抗凝治疗率均≥75%。
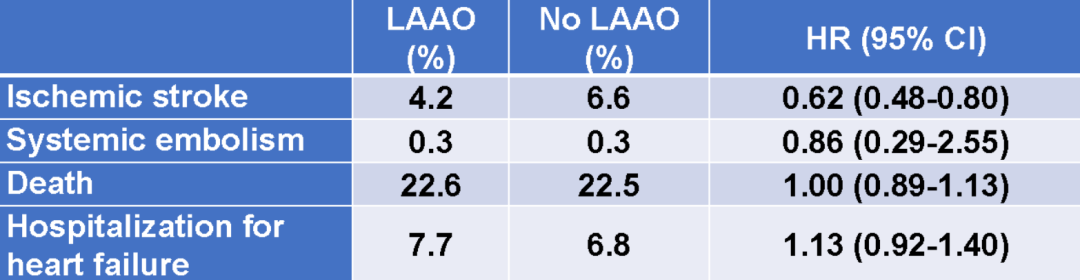
平均随访3.8年后,LAAO组患者首要终点事件风险下降33% (HR 0.67, 95%CI [0.53-0.85], p=0.001)(图1),手术30天后该风险下降达42%(表4)。亚组分析提示,获益更明显的对象包括男性、年龄≥72岁、CHA2DS2-VASc≤4分、瓣膜手术、既往心衰者(图2)。次级终点分析提示,LAAO主要降低了卒中风险达38% (HR 0.62, 95%CI 0.48-0.80)(表5)。
表1. 研究对象基线资料

表2 LAAO组组对照组患者心脏手术类型
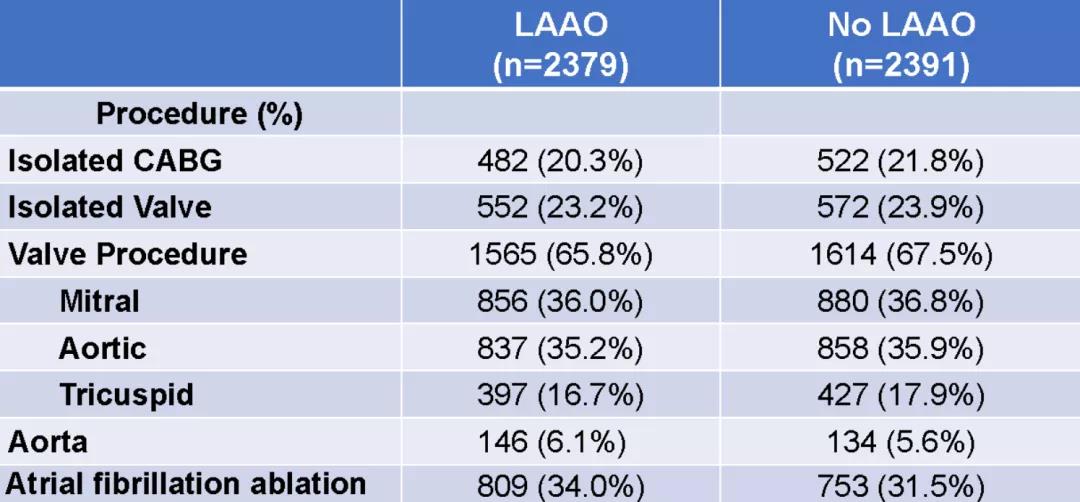
表3. 手术安全结局比较
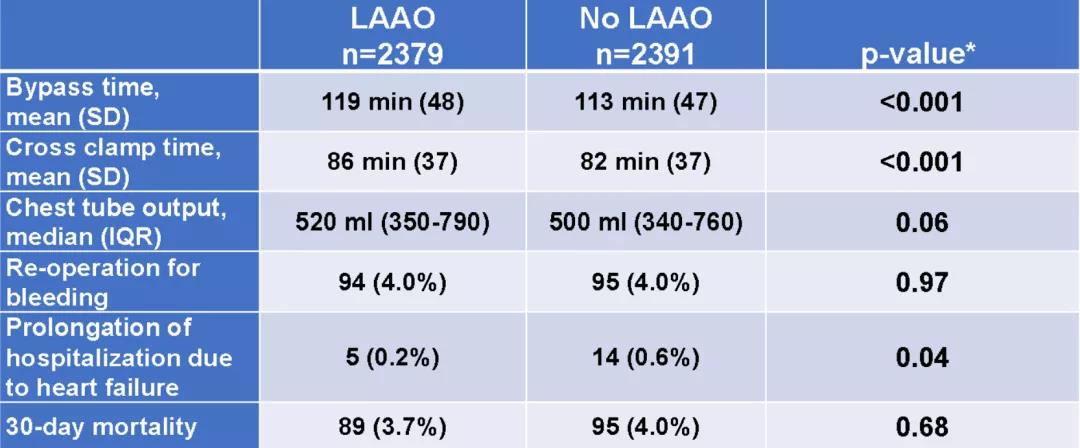
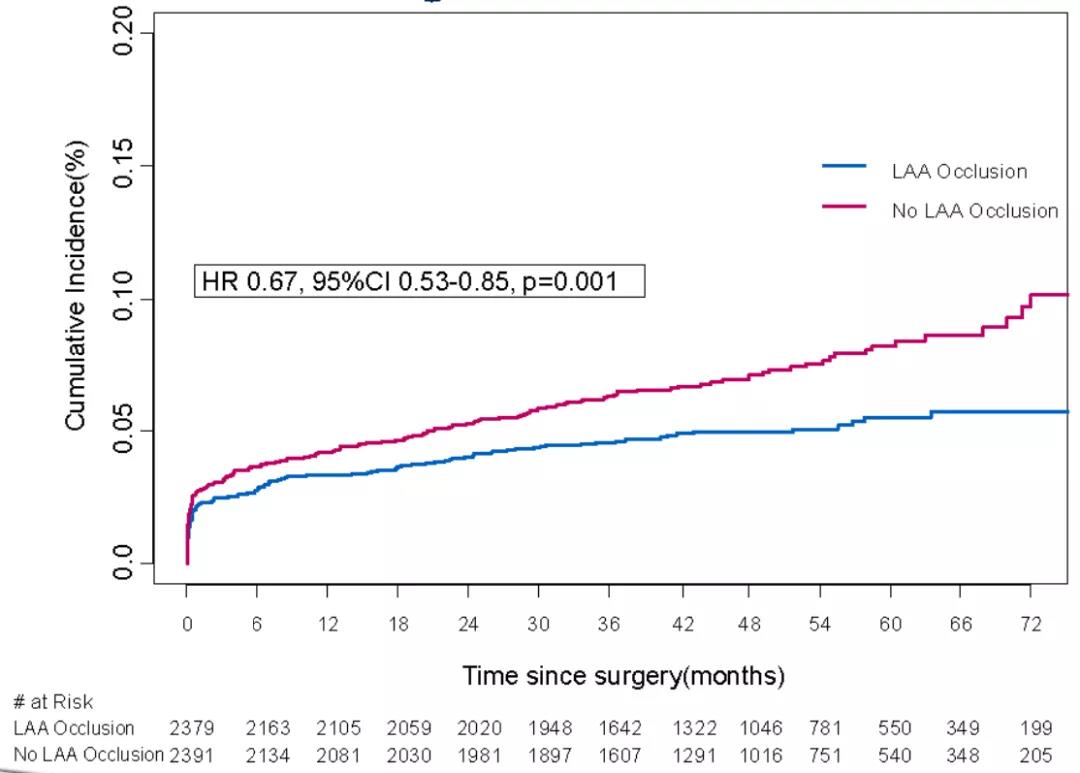
图1. 卒中或系统性栓塞风险比较
表4. 比较随访3.8年首要结局
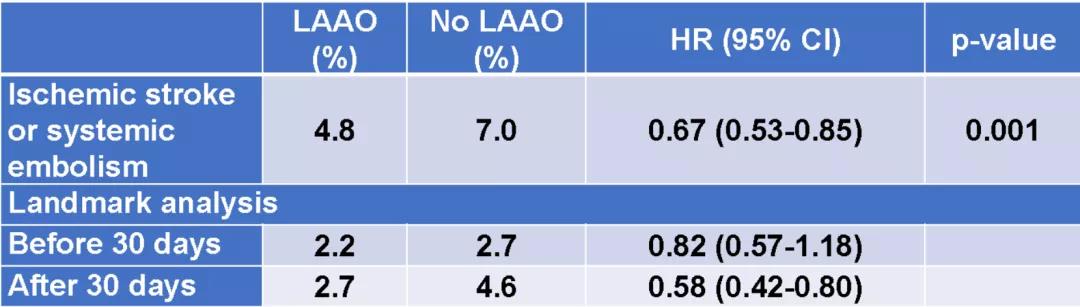
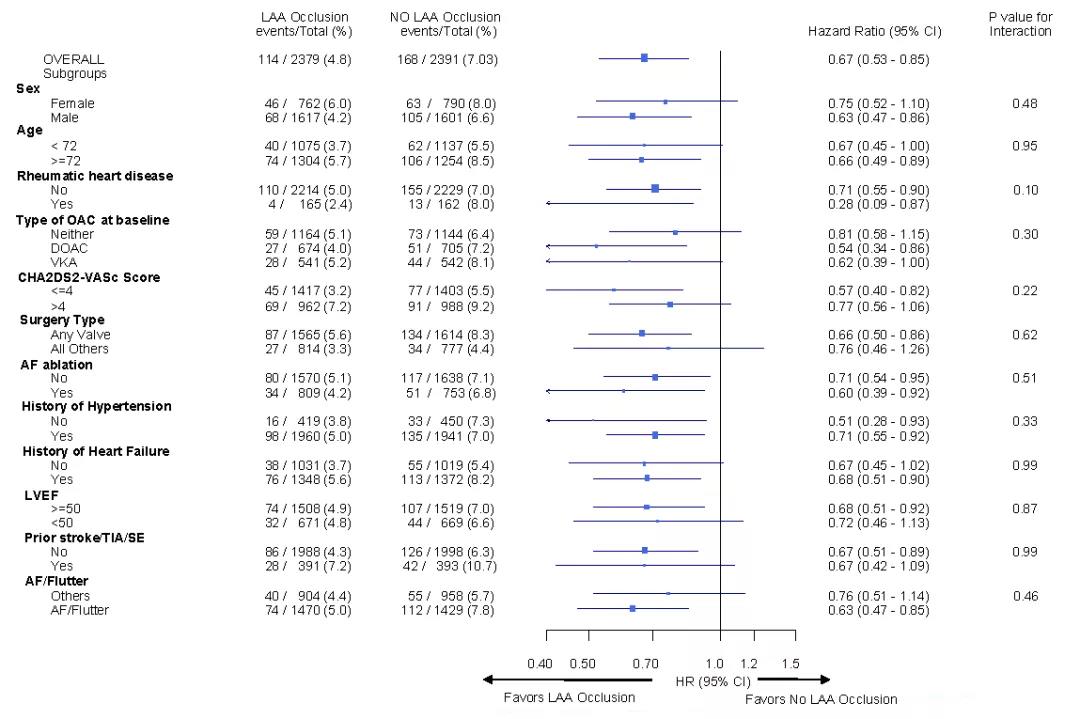
图2. 亚组分析结果
表5. 次级终点分析
研究结论
ACC.21|LAAOS III
外科手术同期行LAAO可降低卒中风险33%,且不增加不良反应风险。该卒中风险的降低独立于口服抗凝药之外。
专家点评
ACC.21|LAAOS III
目前由于众多RCT研究证据支持口服抗凝药预防房颤相关卒中,该策略已成为房颤卒中预防的基石。与前者相比,关于左心耳封堵(LAAO)(内科方式)预防房颤卒中的RCT证据不足,因此指南推荐等级不高。而外科左心耳封堵的证据更加缺乏,指南推荐等级更低,目前仅为IIb类推荐。
此次,LAAOS III研究的发布为该领域进步做出重要贡献,提示在心脏手术时可行同期外科LAAO是安全、有效的,但仍然有许多问题有待回答,如LAAO可否替代口服抗凝药、低危患者治疗策略等。
点评专家:白瑾教授
ACC.21|LAAOS III
白瑾 教授
白瑾,中共党员,医学博士;北京大学第三医院 心内科副主任医师;北医三院机场院区综合内科副主任;专业以心律失常疾病的药物及手术治疗、心脏疾病的康复治疗为重点研究方向;学术兼职:2014年任北京市康复医学会心肺康复分会委员; 2016年任北京医学会心血管病学会分会康复学组委员;2018年任北京大学医学部血管疾病社区防治中心高血压血管病研究专家委员会委员;2019年任中国老年保健医学研究学会老年心血管病分会青年委员;2019年任中国生物医学工程学会心律分会青年委员;2020年任中国人体健康科技促进会高血压防控与研究专业委员会常务委员。从事心血管内科专业以来,作为第一作者发表专业相关研究的国内核心期刊文章10余篇;参与翻译心血管专业书籍4部;参与多项卫生部临床重点项目、北京大学“985”课题和国家“十一五”科技支撑计划课题,以及心血管疾病相关基础研究国家自然科学基金。
作者:李延广
医学博士,北京大学第三医院心内科。英国伯明翰大学心脏科学中心Research Fellow。中国老年医学会老年病学分会委员,中国老年保健医学研究会老年心血管病分会青年委员。Cerebrovascular Disease杂志编辑、审稿人,BMC Neurology杂志审稿人。主要从事心律失常与心电生理临床及研究工作。发表SCI及中文核心期刊论文30余篇。建立了第一个临床型新发心房颤动风险评估模型-C2HEST评分,验证人群超500万,涉及来自韩国、法国、美国、欧洲多种族人群,受到多个国际房颤指南引用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AAO#
118
#III#
88
#LAAO#
96
#AAOS#
87
#ACC#
93
#左心耳#
0
#北医三院#
84
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
95
房颤,临床上碰到很多哦
103