JAHA:血栓抽吸对STEMI患者死亡率、支架内血栓形成和卒中的影响!
2018-01-09 xing.T MedSci原创
由此可见,两组间死亡率无差异。血栓抽吸与降低支架血栓形成风险相关。该研究为先前关于死亡率的随机研究进行外部验证提供了重要证据。
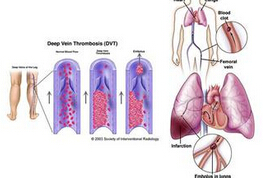
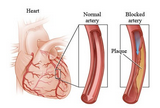
尽管有2个大型随机临床试验结果显示ST段抬高心肌梗死患者行经皮冠状动脉介入治疗时进行常规的血栓抽吸治疗并没有明显效果,但仍有大量患者在使用血栓抽吸这一手段。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该观察性研究使用来自于瑞典冠状动脉造影和血管成形术登记研究(SCAAR研究)所有可用的数据旨在评价血栓抽吸对死亡率、支架内血栓形成和卒中的影响。
研究人员确定了42829例在2005年1月至2014年9月期间连续就诊接受经皮冠状动脉介入治疗的ST段抬高心肌梗死患者,这些患者在SCAAR进行了登记。在25%的手术操作中使用血栓抽吸。研究人员采用工具变量分析法,以行政卫生区域作为治疗偏好工具变量,来评估血栓抽吸对死亡率、支架血栓形成和卒中的影响。
研究人员发现血栓抽吸与30天内(风险降低:-1.2;95%可信区间[CI]为-5.4到3;P=0.57)和1年(风险降低:-2.4;95%CI为-7.6到3;P=0.37)的死亡率无关。血栓抽吸与30天(风险降低:-2.7;95%CI为-4.1到-1.4;P<0.001)和1年(风险降低:-3.5;95%CI为-5.3到-1.7;P<0.001)支架内血栓形成风险降低有关。住院卒中和神经系统并发症在各组之间没有差异(风险降低:0.1;95%CI为-0.8到1.1;P=0.76)。
由此可见,两组间死亡率无差异。血栓抽吸与降低支架血栓形成风险相关。该研究为先前关于死亡率的随机研究进行外部验证提供了重要证据。
原始出处:
Oskar Angerås,et al. Impact of Thrombus Aspiration on Mortality, Stent Thrombosis, and Stroke in Patients With ST‐Segment–Elevation Myocardial Infarction: A Report From the Swedish Coronary Angiography and Angioplasty Registry.JAHA.2017. https://doi.org/10.1161/JAHA.117.007680
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者死亡#
59
#STEMI患者#
59
#血栓抽吸#
68
#支架内血栓#
110
血栓抽吸的作用.
93
#AHA#
57
#STEM#
50
阅
72
很好的文章学习了
76
尽管有2个大型随机临床试验结果显示ST段抬高心肌梗死患者行经皮冠状动脉介入治疗时进行常规的血栓抽吸治疗并没有明显效果.但仍有大量患者在使用血栓抽吸这一手段
79