肝转移性恶性黑色素瘤超声表现1例
2019-05-05 陈云 赵静雯 唐缨 中国超声医学杂志
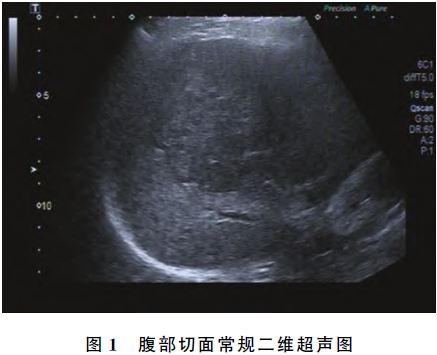
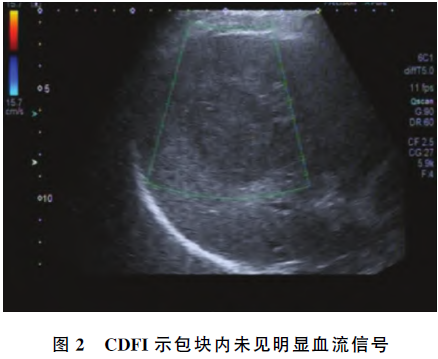
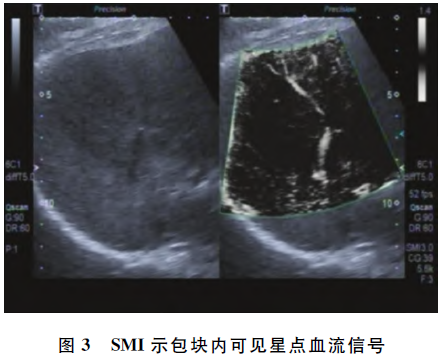
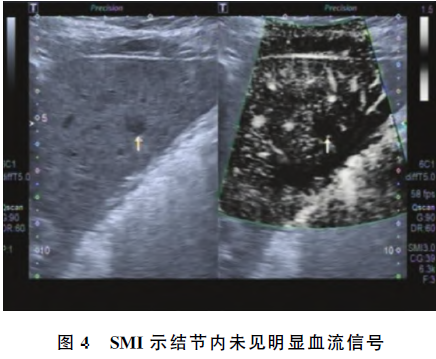
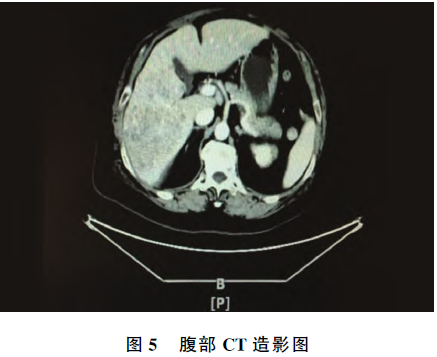
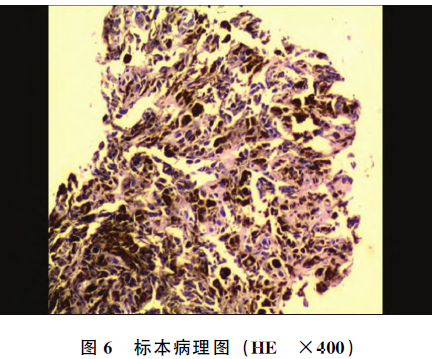
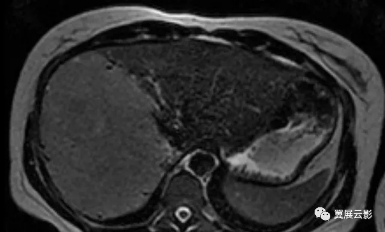
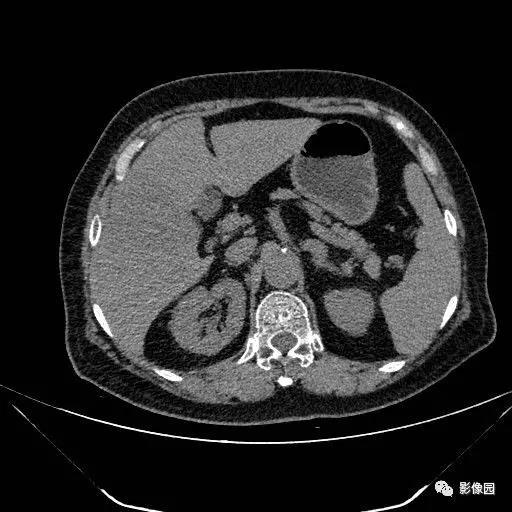
患者女,73岁。主因右侧腹痛1个月余,加重10d入院。既往主因黑色素瘤行右眼眼球摘除术史40余年,高血压病史40余年,腔隙性脑梗死病史20余年,心率过快病史5年余。查体:未见明显异常。血常规:血小板(PLT)395×109/L,淋巴细胞数0.78×109/L,淋巴细胞百分比15.20%,余实验室检查未见明显异常。腹部彩超所见:肝内探及多发低回声病灶,较大位于右叶,大小约10.4 cm×8.3 cm
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#超声表现#
82
#色素#
0
#转移性#
71
#肝转移#
74
#黑色素#
79
#黑色素#
67