下腔静脉连接左心房合并心内畸形二例
2019-07-17 汪青园 黄景思 邹鹏 影像诊断与介入放射学
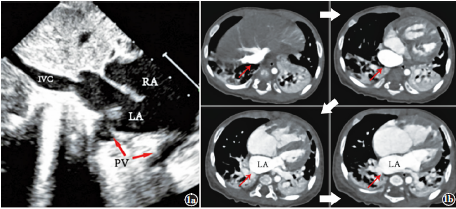
病例1,女,3个月16d。因为生长发育缓慢就诊(出生体重3.15kg,入院体重3.67kg)。呼吸室内空气的情况下,四肢经皮血氧饱和度测量值为97%~100%。体格检查,呼吸48次/分,心前区未闻及明显杂音。心电图提示:窦性心律。胸片提示:右心缘明显膨隆,肺动脉段隆起,肺血增多,心胸比0.57。超声及CT共同提示:下腔静脉连接左心房(图1),心内型部分肺静脉异位引流,继发孔型房间隔缺损,动脉导管未

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#下腔静脉#
97
#左心房#
87
#静脉#
69
#畸形#
63
#心房#
73
学习了,谢谢分享
123