Brit J Cancer:接受阿那曲唑治疗5年的绝经后妇女骨密度变化
2021-01-25 MedSci原创 MedSci原创 发表于上海
这是第一个报告停止阿那曲唑预防乳腺癌患者中BMD变化的研究。该研究的结果表明,阿那曲唑用于预防乳腺癌对BMD的负面影响部分是可逆的。
阿那曲唑治疗期间与显著加速的骨密度(BMD)丢失有关。近日,肿瘤学领域权威杂志British Journal of Cancer上发表了一篇研究文章,研究人员纳入了1410名绝经后妇女,她们被纳入BMD亚组研究,根据她们脊柱或股骨颈的基线T评分得分为三个层次。

这项分析的主要目的是调查那些没有接受二膦酸盐治疗的患者,在停止治疗两年后(第5年至第7年),脊柱和髋关节的双能X线吸收测定法(DXA)测定的BMD是否发生变化。
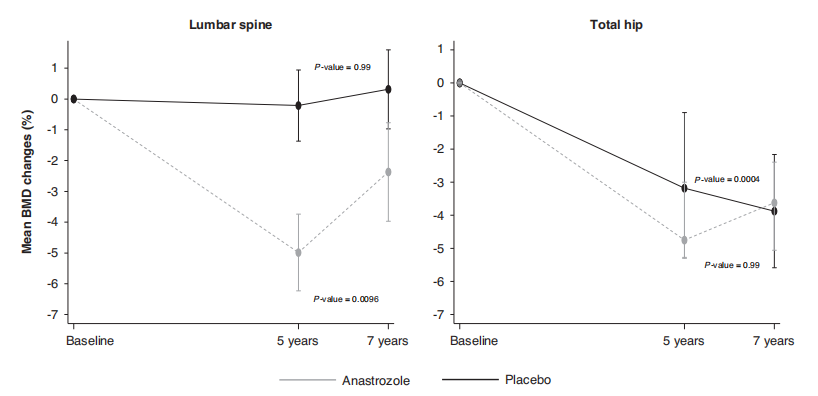
该研究共有528名未接受二膦酸盐治疗的妇女获得了5年和7年的BMD数据。在基线时BMD正常的女性中,研究人员观察到阿那曲唑停药后腰椎BMD增加了1.25% (95%CI为0.73-1.77) (P=0.0004),比安慰剂组增加幅度要大(0.14%(−0.29-0.56))。髋关节方面,服用阿那曲唑组患者的BMD在5-7年间保持不变,而随机分至慰剂组的BMD继续下降(-1.35%(-1.70至-0.98))。
由此可见,这是第一个报告停止阿那曲唑预防乳腺癌患者中BMD变化的研究。该研究的结果表明,阿那曲唑用于预防乳腺癌对BMD的负面影响部分是可逆的。
原始出处:
Ivana Sestak.et al.Off-treatment bone mineral density changes in postmenopausal women receiving anastrozole for 5 years: 7-year results from the IBIS-II prevention trial.Brit J Cancer.2021.https://www.nature.com/articles/s41416-020-01228-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
75
学习中
99
#绝经#
81
#绝经后妇女#
99
#阿那曲唑#
72
#绝经后#
75
学习中
106
学习了
113
了解
109
了解
98