Eur J Cancer:抗PD-1辅助治疗黑色素瘤的真实临床实践数据!
2021-10-07 Nebula MedSci原创
与临床实践相比,在日常实践中,III/IV期黑色素瘤切除后进行抗PD-1辅助治疗显示出略高的毒性率和更高频的提前停药,但无进展生存率相近
黑色素瘤,通常是指恶性黑色素瘤,是黑色素细胞来源的一种高度恶性的肿瘤,简称恶黑,多发生于皮肤,也可见于黏膜和内脏,约占全部肿瘤的3%。皮肤恶性黑色素瘤占皮肤恶性肿瘤的第三位(约占6.8%~20%)。好发于成人,极少见于儿童。
虽然有很多关于黑色素瘤辅助治疗的临床试验,但关于真实临床上接受辅助治疗的黑色素瘤患者预后的数据很少。自2019年起,辅助治疗的黑色素瘤患者会在DMTR(荷兰监测黑色素瘤诊疗质量和安全性的一个以人群为基础的注册处)上注册。
本研究旨在通过DMTR上注册的患者数据来分析实际临床上接受辅助治疗的黑色素瘤患者的治疗模式、复发率和不良事件发生率。
纳入了DMTR上接受过辅助治疗的黑色素瘤患者。采用描述性统计分析患者特征和治疗特征。采用Kaplan-Meier法估计12个月的无复发生存率 (RFS)。
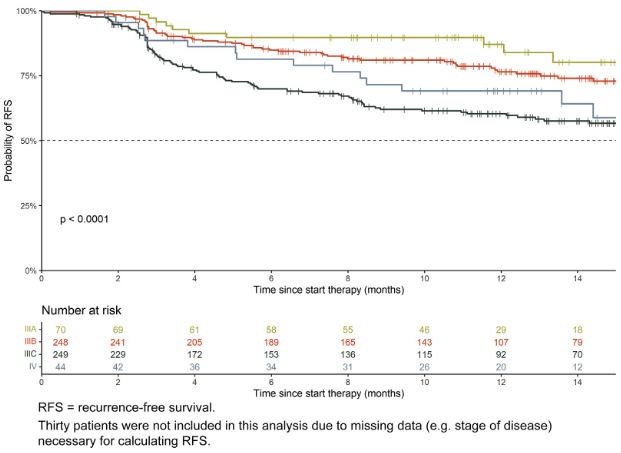
接受抗PD-1辅助治疗的不同分期的黑色素瘤患者的PFS
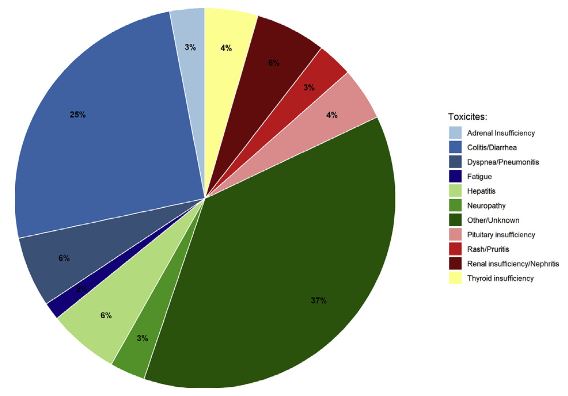
共纳入了641位接受抗PD-1辅助治疗的黑色素瘤患者。中位随访了12.8个月后,12个月的无复发生产率为70.6%(95% CI 66.9-74.6)。性别、疾病分期和Breslow厚度都与RFS的高风险相关。18%的接受抗PD-1治疗的患者发生过3级及以上的毒性反应。61%的患者提前终止了抗PD-1治疗。
抗PD-1治疗期间或治疗后发生的3级及以上的毒性反应
综上所述,与临床实践相比,在日常实践中,III/IV期黑色素瘤切除后进行抗PD-1辅助治疗显示出略高的毒性率和更高频的提前停药,但无进展生存率相近。
原始出处:
de Meza Melissa M,Ismail Rawa K,Rauwerdink Daan et al. Adjuvant treatment for melanoma in clinical practice - Trial versus reality.[J] .Eur J Cancer, 2021, https://doi.org/10.1016/j.ejca.2021.08.044
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#色素#
73
#临床实践#
75
#黑色素#
75
#黑色素#
80