Sci Rep: 活性氧在前列腺癌中可控制基质细胞和癌细胞中MMP-3的表达
2017-08-28 AlexYang MedSci原创
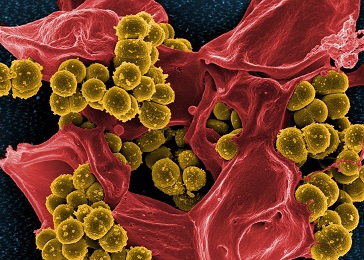
关于细胞外基质(ECMs)间接控制的研究主要集中在恶性肿瘤细胞的作用,而在癌症发展期间基质细胞的作用上关注较少。因此,最近有研究人员通过利用来自共培养细胞模型和临床病人样本的正常和前列腺癌基质细胞(CAFs),阐释了尽管CAFs可以促进前列腺癌的生长,基质金属蛋白酶-3(MMP-3)在CAFs中表达量较低,而在前列腺癌细胞中表达量提高。更进一步的是,研究人员发现过氧化氢通过不同的调控机制,为MMP
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#基质#
72
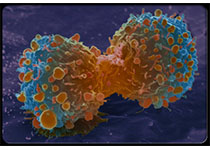
#癌细胞#
59
#活性氧#
96
学习了谢谢分享
91
学习了新知识
101
学习谢谢分享
108
增加了见识不错
85
最后.研究人员表明他们的研究首次阐释了在肿瘤发展过程中.活性氧在基质细胞和前列腺癌细胞中控制MMP-3表达的关键角色.明确了肿瘤微环境是怎样调节ECM的自稳调节.
85
学习了.谢谢分享
104
学习谢谢分享
86