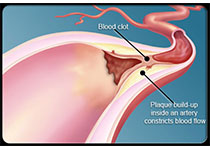
NEJM:巨细胞动脉炎所致舌坏死
2018-07-06 杨中华 脑血管病及重症文献导读
疲劳,头痛和吞咽困难15天。 既往,每天服用阿司匹林。 查体发现可以触及双侧颞动脉明显搏动。无发热或头皮压痛,眼科检查正常。 实验室检查显示白细胞14950/mm3,血沉为120 mm/h。 诊断为巨细胞动脉炎。双侧颞动脉活检,并开始激素治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动脉炎#
83
#坏死#
141
#巨细胞#
112
学习谢谢分享
164
谢谢分享学习
164