BMJ:儿童新冠肺炎患者中,年龄越小后遗症风险越高,恢复期更长
2022-01-18 MedSci原创 MedSci原创
挪威儿童及青少年新冠肺炎患者中,学龄前儿童的后遗症风险较高,需要更长的恢复时间,最常见的后遗症为呼吸系统疾病

研究发现,Covid-19成人在首次感染SARS-CoV-2病毒后仍可能会出现3-6个月的症状,主要是呼吸和循环疾病。虽然儿童新冠肺炎患者的比例较低并且多数症状轻微,但仍有后遗症的风险。最新研究发现,新冠肺炎重症患者康复后后遗症及并发症风险较高,而轻症患者可能出现长期后遗症。近日研究人员考察了新冠肺炎儿童患者康复后的后遗症风险以及医疗保健服务需求。
本次研究在挪威开展,2020年8月1日至202年2月1日期间接受SARS-CoV-2检测(阳性病例10279 人次,阴性275859 )或未检测(n=420747)的1-19岁挪威儿童及青少年参与,按年龄进一步分为1-5岁、6-15岁和16-19岁组。研究的主要终点为核酸检测前后6个月,初级保健(全科医生或急诊)和专科保健(门诊或住院患者)的医疗活动。
在SARS-CoV-2检测结果呈阳性后的第一个月内,与检测结果呈阴性的参与者相比,阳性患儿的初级保健使用率在短期内有显著的相对增加(1-5岁:339%;6-15岁:471%;16-19岁:401%)。在两个月(1-5岁:22%;6-15岁:14%;16-19岁:11%)和三个月(1-5岁:26%,6-15岁:15%;16-19岁:11%)时,年龄稍小组儿童的初级保健率仍显著增加。与检测呈阴性的1-5岁儿童相比,阳性儿童在长达6个月内,初级保健率仍相对增加(13%),这一情况在较年长年龄组中没有观察到。对于所有年龄组,初级保健就诊人数的增加是由于呼吸系统不适造成的。没有观察到专科就诊率的显著增加。
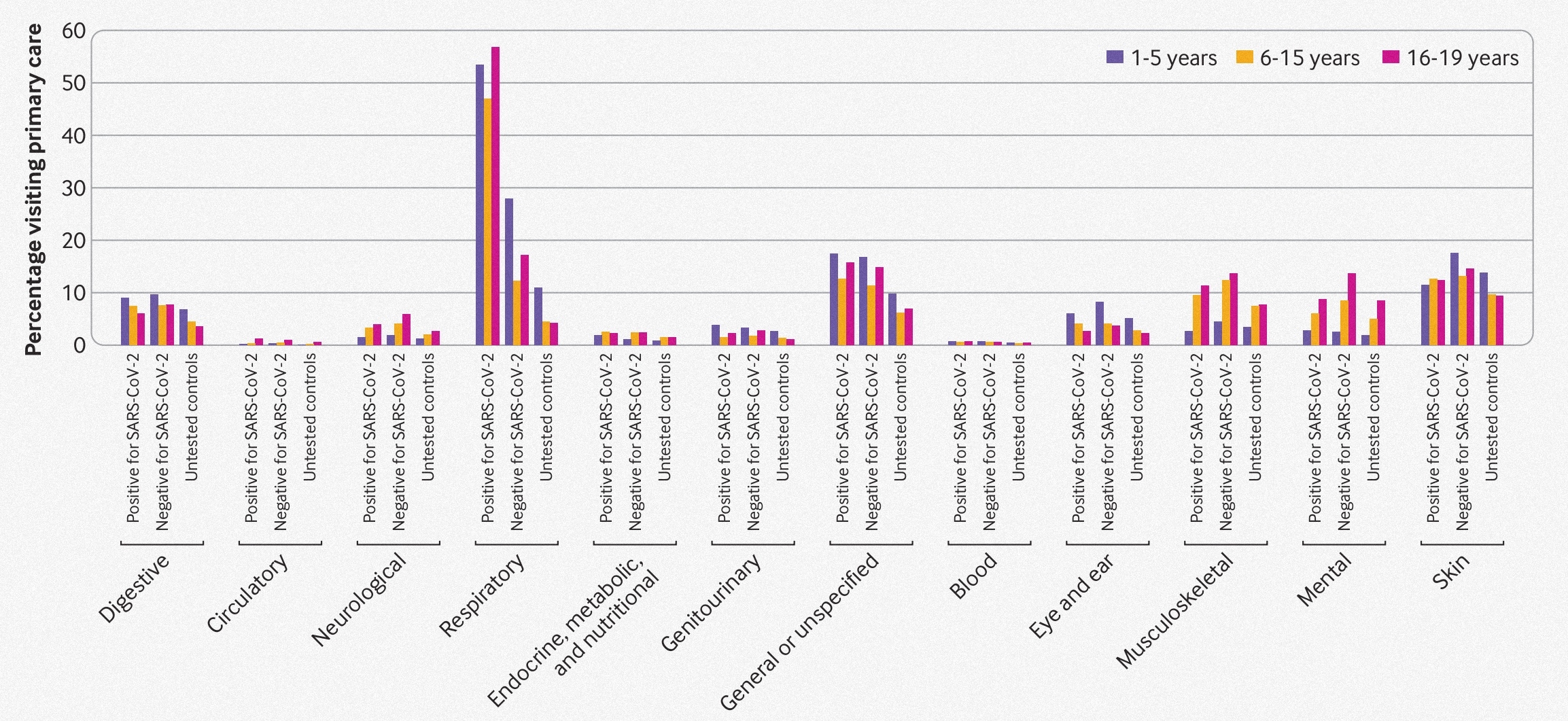
新冠肺炎患儿后遗症就诊情况
研究发现,挪威儿童及青少年新冠肺炎患者中,学龄前儿童的后遗症风险较高,需要更长的恢复时间,最常见的后遗症为呼吸系统疾病。
原始出处:
Karin Magnusson et al. Healthcare use in 700 000 children and adolescents for six months after covid-19: before and after register based cohort study. BMJ,17 January 2022。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
77
#恢复期#
112
#后遗症#
109
学习啦
122
学习到了新知识
112
不错,学习了
131