Nature:基因组错误折叠或提供新的癌症研究思路
2015-12-28 佚名 生物谷
近日,发表在Nature杂志上的一篇研究论文中,来自麻省总医院和博德研究所的科学家揭示了隐藏在癌症背后的一种新型生物学机制,文章中,通过对携带异柠檬酸脱氢酶基因(IDH)突变的脑瘤进行研究,研究者揭开了指导基因组自身折叠指令的罕见改变,这些指令改变可以靶向作用基因组的关键部分—绝缘子,绝缘子可以抑制某个区域的基因同控制开关及附近区域的特殊基因发生相互作用,当这些绝缘子在IDH突变的肿瘤中“胡作非为
近日,发表在Nature杂志上的一篇研究论文中,来自麻省总医院和博德研究所的科学家揭示了隐藏在癌症背后的一种新型生物学机制,文章中,通过对携带异柠檬酸脱氢酶基因(IDH)突变的脑瘤进行研究,研究者揭开了指导基因组自身折叠指令的罕见改变,这些指令改变可以靶向作用基因组的关键部分—绝缘子,绝缘子可以抑制某个区域的基因同控制开关及附近区域的特殊基因发生相互作用,当这些绝缘子在IDH突变的肿瘤中“胡作非为”时,期就会促进一系列生长因子基因被基因开关所控制,最终形成强大的促癌组合,相关研究货位后期开发新型的抗癌疗法提供思路。
研究人员Bradley Bernstein表示,我们揭示了癌症发生的一种机制,而且我们认为这种机制不仅仅存在于脑瘤中;如今科学家们可以确定促癌基因会通过DNA序列的改变而出现异常的激活,而在本文中研究人员则发现,促癌基因会通过基因组折叠的改变来被开启。
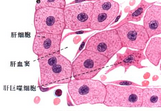
这项研究中,研究人员对神经胶质瘤进行了深入研究,神经胶质瘤是一种脑癌,当然其还包括恶性的胶质母细胞瘤,在过去20年里治疗这种恶性脑瘤的疗法并没有太大进展,因此为了解开这种脑瘤的发生机制,研究者Bernstein就同其同事对近年来癌症基因组的大量数据进行分析,他们检测了IDH突变的肿瘤的发展趋势,当名为PDGFRA的生长因子基因被开启时,远端基因FIP1L1就会被开启,而PDGFRA被关闭时,FIP1L1基因也会被关闭。
很长一段时间以来,IDH突变的肿瘤发生的机制并没有被很好地分析,IDH基因可以编码一种特殊酶类,当其突变后就会产生一种毒性的代谢产物,进而干扰其它不同种类蛋白质的产生,然而具体是什么机制改变引发了癌症研究人员并不清楚。研究者发现,基因组上的绝缘子可以通过多种蛋白的作用进行结合,随后结合到基因组中名为CTCF的区域。
文章中,利用多种基因组尺度的方法进行结合,研究者发现,在IDH突变的神经胶质瘤中,超甲基化可以在CTCF区域集中,结合他们早期的研究成果,他们发现,PDGFRA和FIP1L1在正常情况下处于不同的结构域中,而且几乎不会发生相互作用,但二者在IDH突变的肿瘤中却是关系比较密切的,这种不寻常的关系往往是超甲基化所引起的。
最后Bernstein说道,携带IDH突变的肿瘤还有很多,比如白血病、结肠癌、膀胱癌等等,本文研究为后期进行多种癌症发病机理的研究都提供了新的线索和研究数据。
原始出处:
William A. Flavahan, Yotam Drier,et al. Insulator dysfunction and oncogene activation in IDH mutant gliomas.Nature.23 December 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
76
这篇文章有一定深度
157
是一篇不错的文章
70
太深奥了
133
赞一个
142
#癌症研究#
52
挺复杂
197
不错哦
122
赞一个
135
强
125