CLIN CANCER RES:顺铂耐药的卵巢癌中存在有丝分裂退出异常
2018-09-30 MedSci MedSci原创
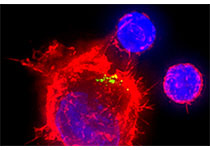
顺铂获得性耐药是成功治疗各种癌症的主要障碍。了解顺铂耐药肿瘤细胞特有的有丝分裂机制可为开发靶向有丝分裂的新型疗法提供基础。CLIN CANCER RES近期发表了一篇文章研究这一问题。
原始出处:
Anil Belur Nagaraj, Olga Kovalenko,et al. Mitotic Exit
Dysfunction through the Deregulation of APC/C Characterizes Cisplatin-Resistant
State in Epithelial Ovarian Cancer.CLIN CANCER RES.September 2018 doi: 10.1158/1078-0432.CCR-17-2885
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#顺铂耐药#
103
#铂#
75
#有丝分裂退出#
63
#有丝分裂#
77