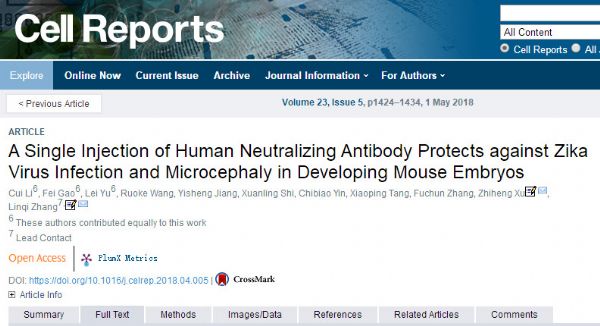
Mol Ther:上海药物所发现整合素aIIbβ3的种属差异与单抗诱导的血小板减少症相关
2018-05-29 上海药物所 中国生物技术网
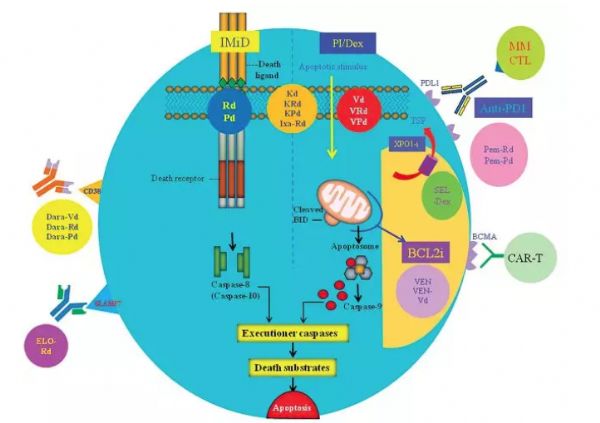
在目前世界范围内,治疗性单克隆抗体(Monoclonal antibodies,mAbs)销售额已达数百亿美元,占到整个生物制药市场份额的三成以上。虽然大部分mAbs在人体中能够良好地耐受,但也依然会造成包括免疫反应、感染性疾病、自身免疫疾病、血小板减少、血栓形成障碍、皮炎及心血管毒性等毒副作用。因此,如何在药物研发前期尽早地发现mAbs造成的不良反应显得极为重要。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#上海药物所#
82
学习了.谢谢作者分享!
103
#血小板减少#
70
#整合素#
82
了解一下
105
了解一下.谢谢分享!
95
好文.值得点赞!认真学习.应用于实践!谢谢分享给广大同好!
128