Int J Cardiol:成年先天性心脏病患者心源性猝死的发生率及临床特点!
2017-12-07 xing.T MedSci原创
由此可见,成年CHD患者发生SCD的风险仍然较高,尤其是存在复杂的基础性缺陷患者。中等到高风险病变包括艾森门格综合征、完全性大动脉转位(心房调转术或先天性矫正)和Fontan循环。
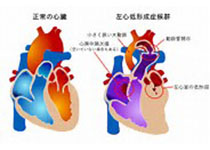
近几十年来,患有先天性心脏病(CHD)的成年人的预期寿命有了很大的提高,非心血管死亡原因现在与传统的心血管疾病差别不大。心源性猝死(SCD)这一灾难性事件的风险CHD患者仍然高于一般人群。
近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员回顾了2935例成年CHD患者数据库(年龄≥16岁)并记录了2000年至2015年期间所有的SCD病例。研究人员确定了先天性缺陷和复杂性疾病所致的SCD发病率和特征。
研究人员记录了35例SCD患者,其发病率为0.4人死亡/1000患者每年。简单、中等和复杂的先天性疾病发生率分别为0.04/1000、0.57/1000和2.0/1000患者每年。风险最高的类型为艾森曼格综合征,为4.8人死亡/1000患者每年。中等风险的病变包括完全性大动脉转位(心房调转术或先天性矫正)和Fontan循环。修复后的法洛四联症、房间隔缺损和左心室流出道损伤均为风险较低的病变。研究人员观察到SCD患者房性心律失常(43%)和QRS波延长(平均为132ms)的患病率均较高。
由此可见,成年CHD患者发生SCD的风险仍然较高,尤其是存在复杂的基础性缺陷患者。中等到高风险病变包括艾森门格综合征、完全性大动脉转位(心房调转术或先天性矫正)和Fontan循环。
原始出处:
Benjamin Moore, et al. Incidence and clinical characteristics of sudden cardiac death in adult congenital heart disease.International Journal of Cardiology.2017. https://doi.org/10.1016/j.ijcard.2017.11.117
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发生率#
107
#临床特点#
71
#Cardiol#
112
学习并分享!!
156
#先天性#
80
#心源性#
63
学习并分享!!
108
好
100