本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

2017-10-10 欧阳沐 生物通
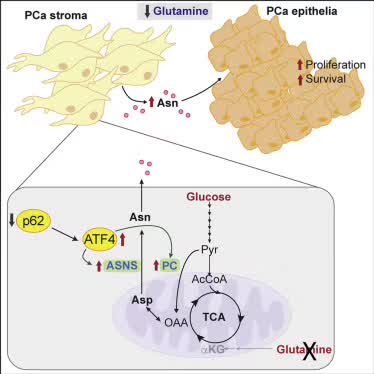
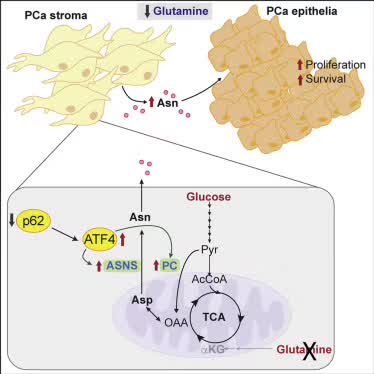
最新《Cell Metabolism》文章,间质组织ATF4途径可能是破坏肿瘤供应链的新靶标。

恶性肿瘤的规范治疗很重要,也可以说肿瘤的治疗没有回头路,首诊方案制定不合理,后期想要挽回困难很大。作为国内众多肺癌领域的知名专家之一,李峻岭教授积极倡导在指南指导下的肺癌个体化治疗策略,倡导多学科合作的综合治疗,以图在现有条件下最大限度的延长患者生存时间,改善生活质量,顾及治疗经济学。很多华人回国治肺癌门诊现场:王先生拿着母亲资料来李教授门诊复查,“李教授,我母亲是否需要在治疗之余吃一些中药或
10所委委属(管)医院与12所河北省对口医院合作,提升心血管、肿瘤、生殖医学等专科和学科技术水平。
上海交通大学医学院附属仁济医院妇产科主任医师王育教授日前成功为一位孕14周的孕妇切除重达3455g的巨大肿块,同时也保住了孕妇子宫内14周的胎儿。术后10天患者顺利出院,母胎平安。
麻省理工学院的生物学家已经发现了一种帮助脑肿瘤称为胶质母细胞瘤积极发展的基本机制。 在小鼠中阻断这种机制后,研究人员能够阻止肿瘤生长。
癌症研究者们一直称赞p53肿瘤抑制蛋白,因为它拥有防止不守规矩的细胞形成肿瘤的能力。但是P53非常善于隐藏自己的卓越功能。
2017年9月26日-30日,备受业内瞩目的“第20届全国临床肿瘤大会暨2017年CSCO学术年会”在厦门隆重开幕。本届年会以“传承创新,携手同行”为主题,并继续秉承CSCO的根本宗旨,开展了多种形式的继续教育和学术交流活动。梅斯小编为大家带来现场报道。在此次大会上,来自中国空军医院的中国抗癌协会肿瘤临床协作中心(CSCO)会员——王颖杰教授围绕“肿瘤放疗所致血小板减少的治疗策略”分享了自己的看法


梅斯医学MedSci APP
医路相伴,成就大医
#Cell#
64
#CEL#
73
#Meta#
79
学习了谢谢分享!!
118
内容丰富.值得学习
92
学习了谢谢了'
123
#MET#
88