J Thromb Haemost:高风险抗磷脂综合征患者血小板减少症!
2018-01-09 xing.T MedSci原创
该研究结果显示高危APS患者血小板减少症患病率较低。在所有恶化为灾难性疾病的患者中均可观察到血小板计数下降。高危APS患者血小板计数下降应被视为疾病进展至CAPS的警示信号。
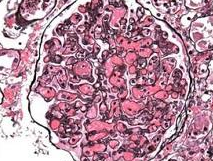
血小板减少症是抗磷脂综合征(APS)患者最常见的非标准性血液学特征。这种疾病在严重APS(CAPS)中更常见。近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,研究人员评估了一系列APS高危患者血小板减少症的患病率,并且评估CAPS患者血小板计数的情况。
这是一项横断面研究,研究人员分析了同组高危APS患者(三联症阳性)的血小板计数。其中6名患者发展为疾病的灾难性阶段,并在发病前、急性期和恢复期记录了血小板计数。
119名高危三联症阳性患者平均血小板计数为210×109/L。考虑到血小板减少症的临界值为100×109/L,血小板减少症的患病率为6%(7例患者)。研究人员发现主要APS和次要APS之间没有差异。在CAPS患者中,血小板计数从基础(212×109/L±51)到诊断时(60×109/L±33)显著下降。完全缓解时血小板计数恢复正常(220×109/L±57)。血小板计数下降总是先于整个临床情况变化。
该研究结果显示高危APS患者血小板减少症患病率较低。在所有恶化为灾难性疾病的患者中均可观察到血小板计数下降。高危APS患者血小板计数下降应被视为疾病进展至CAPS的警示信号。
原始出处:
E Pontara,et al. Thrombocytopenia in high-risk patients with Antiphospholipid Syndrome.Journal of Thrombosis and Haemostasis.2018.http://onlinelibrary.wiley.com/doi/10.1111/jth.13947/full
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#高风险#
63
#HAE#
90
#血小板减少#
83
#综合征#
90