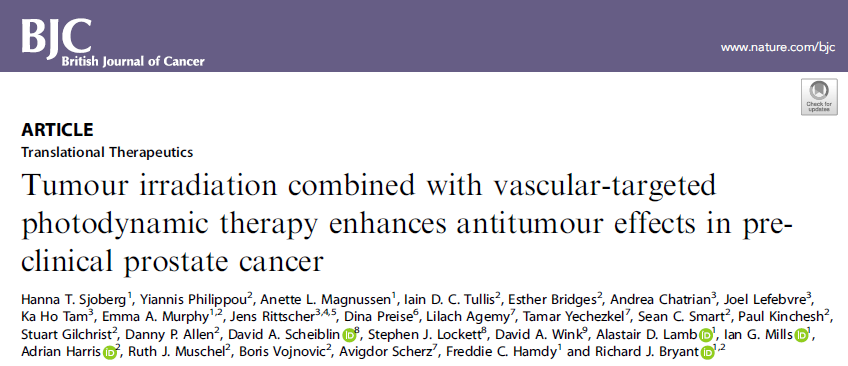
Br J Cancer:分次放疗联合血管靶向光动力疗法可增强对前列腺癌的抗肿瘤作用
2021-06-23 xiaozeng MedSci原创
分次放疗(FRT)联合雄激素剥夺疗法(ADT)是前列腺癌(PCa)的一种治疗选择,然而,三分之一的患者会出现复发,且患者后续的治疗选择有限。
分次放疗(FRT)联合雄激素剥夺疗法(ADT)是前列腺癌(PCa)的一种治疗选择,然而,三分之一的患者会出现复发,且患者后续的治疗选择有限。
此外,FRT和ADT具有显著的副作用。根治性手术(前列腺切除术)是PCa的另一种治疗选择,但也同样有显著的副作用。因此,急需制定改善PCa治疗结果和减少治疗副作用的治疗策略。
血管靶向光动力疗法(VTP)是一种新型的微创局部消融外科手术,其主要是通过自由基介导的快速破坏肿瘤血管系统来实现的。VTP可有效用于低风险小体积的PCa的局部消融,并已被作为放疗复发PCa的一种挽救疗法。
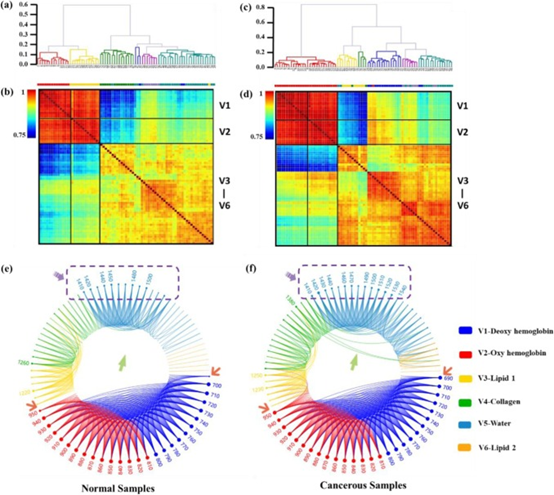
肿瘤血管系统的特征在于血管不成熟、渗透性增加、异常的分支以及低效的流动。FRT能够改变肿瘤微环境并促进短暂的“血管正常化”。在该研究中,研究人员假设,相比于FRT或VTP的单独治疗,二者联合的多模式治疗可以改善对PCa的控制。
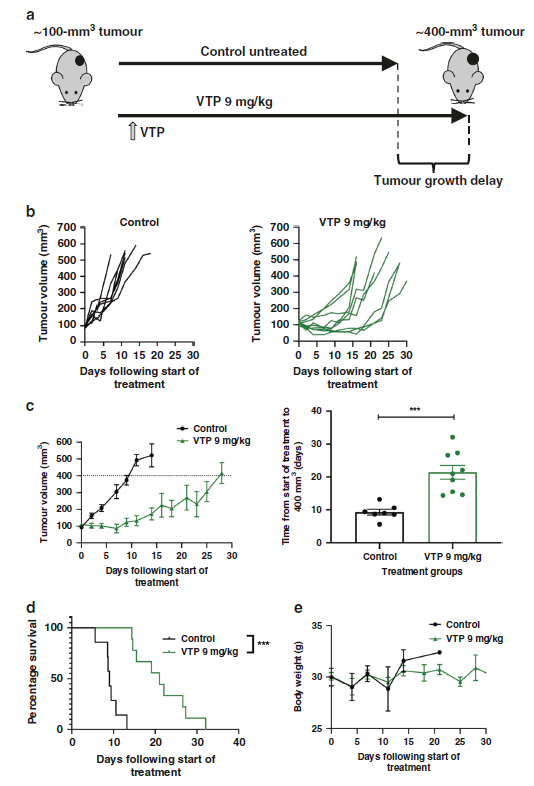
VTP会导致移植瘤的生长延迟
研究人员在临床前PCa模型中研究了该假设,分析连续递送FRT和7天后的VTP治疗是否能够改善对TRAMP-C1 PCa侧翼移植瘤的控制。
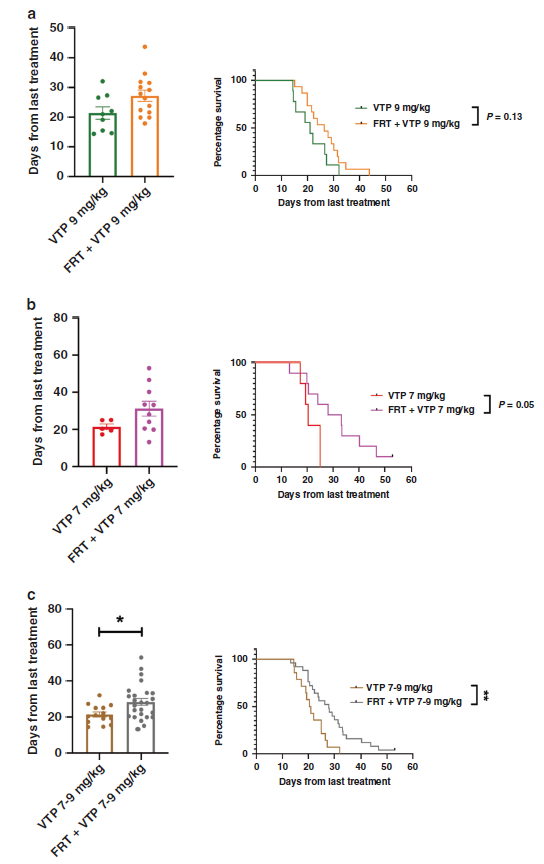
结果显示,FRT能够诱导PCa侧翼移植瘤中的“血管正常化”变化,并改善相关血管功能,而相比于FRT或VTP的单独治疗,FRT后联合VTP治疗能够显著延迟移植瘤模型中的肿瘤生长,并提高总生存率。
新辅助FRT联合7天后VTP治疗可提高患者的疗效
总而言之,该研究结果揭示,FRT和VTP的联合治疗或可成为PCa治疗中的一种具有潜力的多模式治疗策略。这也为该多模式治疗策略提供了概念验证,为后续的早期临床试验提供一定的理论基础。
原始出处:
Sjoberg, H.T., Philippou, Y., Magnussen, A.L. et al. Tumour irradiation combined with vascular-targeted photodynamic therapy enhances antitumour effects in pre-clinical prostate cancer. Br J Cancer (21 June 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#光动力#
100
学习学习
93
好文章,谢谢分享。
82
前列腺癌相关研究,学习了,谢谢梅斯
76