中心点: 第3年时,A+AVD疗法展现出明显优于ABVD疗法的效果,且与PET2状态无关。 在预先指定的亚组中也观察到了A+AVD疗法相对于ABVD疗法的收益,
2020-01-23 QQY MedSci原创
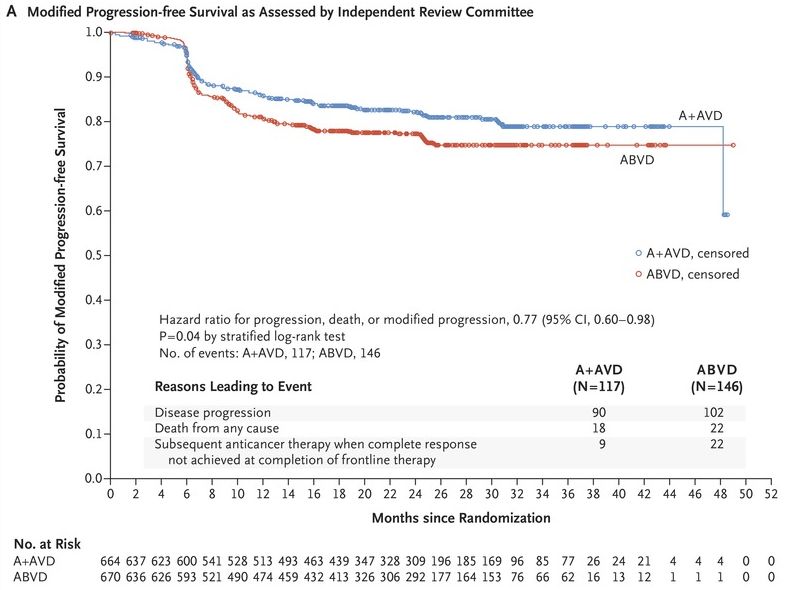
中心点:第3年时,A+AVD疗法展现出明显优于ABVD疗法的效果,且与PET2状态无关。在预先指定的亚组中也观察到了A+AVD疗法相对于ABVD疗法的收益,且与疾病分期、年龄和预后风险评分无关。摘要:3期ECHELON-1研究证实与ABVD作为III/IV期经典霍奇金淋巴瘤(cHL)的一线治疗方法相比,本妥昔单抗(A)联合AVD(A+AVD)疗法可获得卓越的校正PFS。正电子发射断层摄影(PET)
第3年时,A+AVD疗法展现出明显优于ABVD疗法的效果,且与PET2状态无关。
在预先指定的亚组中也观察到了A+AVD疗法相对于ABVD疗法的收益,且与疾病分期、年龄和预后风险评分无关。
摘要:
3期ECHELON-1研究证实与ABVD作为III/IV期经典霍奇金淋巴瘤(cHL)的一线治疗方法相比,本妥昔单抗(A)联合AVD(A+AVD)疗法可获得卓越的校正PFS。正电子发射断层摄影(PET)适应性试验的成熟数据突出了PET适应性方法的潜在局限性,包括剂量强化的毒性和PET2(+)患者高于预期的复发率。本研究为ECHELON-1研究的升级版,包括对每位研究者的3年PFS进行探索性分析。
共1334位III/IV期cHL患者被随机分至6个疗程的A+AVD组(664位)或ABVD组(670位)。2个疗程后予以一次PET扫描(中间PET)。
中位随访37个月时,A+AVD组和ABVD组的3年PFS率分别为83.1%和76.0%;60岁以下的PET2(+)患者的3年PFS率分别为87.2%和81.0%。在采用A+AVD治疗的60岁以下的PET2(+)患者中,也观察到了有益的趋势,3年PFS率为69.2%(ABVD治疗的为54.7%)。
在意向治疗人群中,A+AVD治疗的有益趋势似乎与疾病分期以及预后风险因素无关。在持续随访过程中,78%的采用A+AVD治疗的周围神经病变(PN)患者获得了完全缓解或改善(ABVD治疗的为83%)。
该研究表明,与ABVD相比,A+AVD疗法作为III/IV期cHL患者的一线疗法提供了持久的疗效优势,这在重要的亚组中是一致的,且与PET2的患者状态无关,不需要强化治疗或添加博莱霉素。
原始出处:
David J. Straus, et al.Brentuximab vedotin with chemotherapy for Stage III/IV classical Hodgkin lymphoma: 3-year update of the ECHELON-1 study.Blood. JANUARY 16, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ABVD#
69
#PE#
48
#PET#
82
#AVD#
84
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
63