NEJM:血管内治疗联合溶栓用于大面积急性脑卒中患者
2022-04-07 zhangfan MedSci原创
对梗死面积较大的大血管闭塞急性脑卒中患者接受溶栓联合血管内治疗对改善患者预后的效果优于单纯溶栓,但颅内出血风险增加
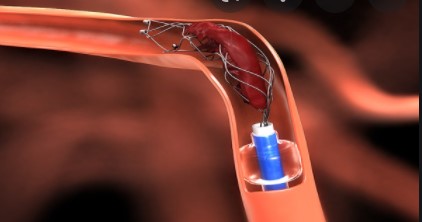
血管内治疗已成为大血管闭塞引起的急性脑卒中的标准治疗手段之一。指南建议,当脑动脉或颈内动脉的M1主干闭塞,且成像显示梗死面积适中(ASPECTS得分6以上)或缺血核心体积和灌注延迟区域间体积不匹配时,应考虑进行血管内治疗。血管内治疗一般不适用于大面积梗死患者。近日研究人员考察了在大面积梗死患者中,血管内治疗联合常规护理的临床效果。
研究在日本开展,早期CT评估ASPECTS得分3到5的脑血管闭塞中风患者参与研究,所有患者在阿替普酶(0.6mg/Kg)治疗基础上,随机接受血管内治疗或对照。研究的主要终点为90天改良Rankin得分0-3的患者比例,次要终点为90天改良Rankin评分结果向好,48小时NIHSS得分改善至少8分的患者比例。
203名患者参与研究,其中血管内治疗组101人,对照组102人,各组均有27%的患者接受了阿替普酶。血管内治疗组31.0%的患者在90天时Rankin得分0-3,对照组为12.7%(RR=2.43)。
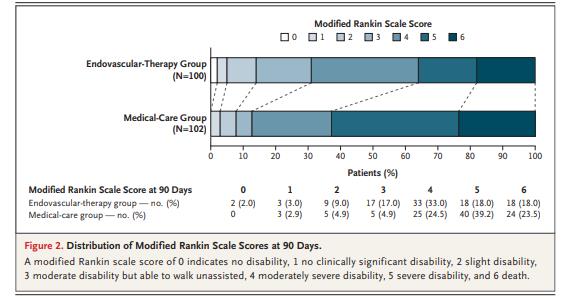
组间90天改良Rankin评分
血管内治疗组90天改良Rankin评分结果向好的患者比例更高。血管内治疗组48小时NIHSS得分改善至少8分的患者占31.0%,对照组仅8.8%(RR=3.51)。颅内出血的发生率分别为58.0%和31.4%。
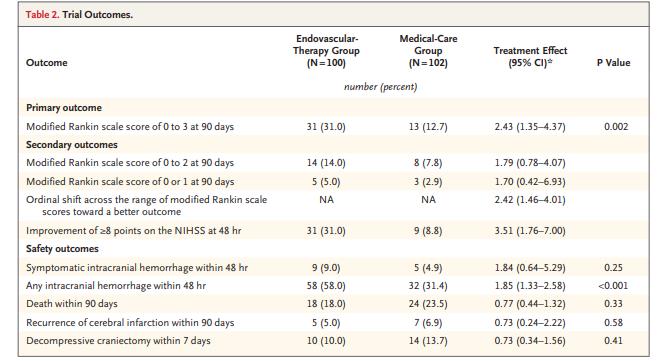
组间临床终点结果差异
研究认为,对梗死面积较大的大血管闭塞急性脑卒中患者接受溶栓联合血管内治疗对改善患者预后的效果优于单纯溶栓,但颅内出血风险增加。
原始出处:
Shinichi Yoshimura et al. Endovascular Therapy for Acute Stroke with a Large Ischemic Region. N Engl J Med,April 7, 2022。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#卒中患者#
89
#大面积#
75
#脑卒中患者#
92
哇喔
107
#急性脑卒中#
86
NEJM上果然牛,感谢梅斯更新及时
88