JCEM:叶切除术会增加甲状腺乳头状癌复发风险?
2016-10-23 MedSci MedSci原创
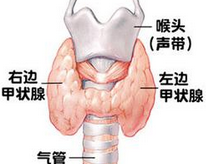
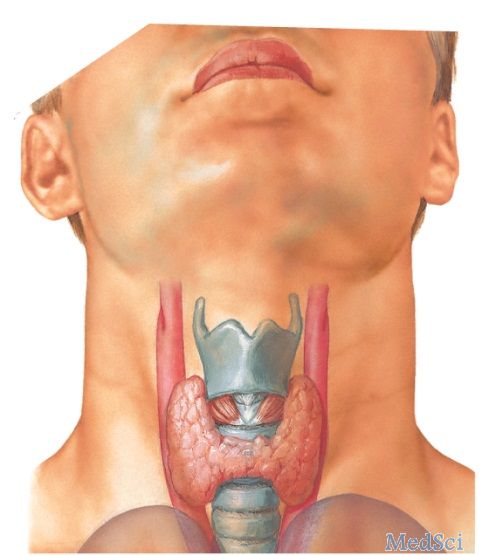
研究数据显示,对于小乳头状甲状腺癌成年患者,接受叶切除术或肿瘤直径至少1.8 cm,两个或两个以上转移性淋巴结或双侧肿瘤,患者的长期复发风险增加。 韩国国立首尔大学医学院的Ka Hee Yi博士和同事进行了一项全国性的、回顾性、多中心研究,包括3282名(平均年龄47岁)甲状腺乳头状癌成年患者,肿瘤直径不超过2 cm。 平均随访5.8年。评估与长期复发相关的高危因素。 总的来说,
研究数据显示,对于小乳头状甲状腺癌成年患者,接受叶切除术者或肿瘤直径至少1.8 cm,两个或两个以上转移性淋巴结或双侧肿瘤,患者的长期复发风险增加。
韩国国立首尔大学医学院的Ka Hee Yi博士和同事进行了一项全国性的、回顾性、多中心研究,包括3282名(平均年龄47岁)甲状腺乳头状癌成年患者,肿瘤直径不超过2 cm。
平均随访5.8年。评估与长期复发相关的高危因素。
总的来说,86%的患者进行了近全或次全甲状腺切除术,77.4%的患者进行了放射性碘消融治疗。
基于肿瘤大小从0.7 cm到1.9 cm,将患者分为两组。为预测复发的风险,肿瘤直径最佳值为1.8 cm。
随访过程中190例患者复发。5年复发率为4.5%,10年复发率为8.9%。
叶切除术组患者与全甲状腺切除术组患者相比,5年和10年的复发率均更高。
最常见的复发部位是颈部淋巴结(64%),其次是甲状腺床和肺。
与长期复发风险相关的因素还有:年龄超过45岁(HR = 0.74; 95% CI, 0.55-0.98),肿瘤直径至少1.8 cm(HR = 2.39; 95% CI, 1.75-3.33),淋巴结转移和接受叶切除术(HR = 1.71; 95% CI, 1.19-2.45)。
原始出处:
Lobectomy may increase recurrence in small papillary thyroid cancer.Healio.October 18, 2016
Hwangbo Y, et al. Long-term Recurrence of Small Papillary Thyroid Cancer and Its Risk Factors in a Korean Multicenter Study.J Clin Endocrinol Metab. 2016;doi:10.1210/jc.2016-2287.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
57
#JCEM#
44
#JCE#
67
#乳头状#
51
#复发风险#
58
#甲状腺乳头状癌#
64