Clin Oral Investig:等离子体处理可提高骨移植材料的表面润湿性
2020-09-29 MedSci原创 MedSci原创
骨移植材料的骨传导性代表了牙周病学和口腔外科领域骨缺损治疗的一个研究领域。从物理化学方面来看,移植材料的湿润性是新骨形成的最重要因素之一。众所周知,氩气等离子体处理(PAT)和紫外线照射(UV)可以增
骨移植材料的骨传导性代表了牙周病学和口腔外科领域骨缺损治疗的一个研究领域。从物理化学方面来看,移植材料的湿润性是新骨形成的最重要因素之一。众所周知,氩气等离子体处理(PAT)和紫外线照射(UV)可以增加材料的表面湿润性,从而提高骨移植的再生潜力。因此,本研究旨在评价PAT和UV处理对各种骨移植物的成骨潜力的影响,其结果已在线发表于Clin Oral Investig。

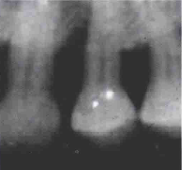
研究选择了以下4种常用的骨移植物:合成羟基磷灰石(Mg-HA)、双相磷酸钙(BCP)、松质和皮质异生骨基质(CaBM、CoBM)。每种移植材料使用66个序列编号的直径10mm的圆盘,并随机分配到以下三组:试验1(PAT)、试验2(UV)和对照(不处理)。六个样品在处理前和处理后使用SEM扫描以评估表面形貌/特征的变化。此外,在利用生物反应器的三维培养系统中培养后,分别在2小时和72小时评价细胞粘附性和细胞增殖。此外,通过测量24小时后人类巨噬细胞的活力,评估PAT和UV对免疫细胞的影响。
SEM分析表明,商业生物材料的初始形态各不相同(如Mg-HA和BCP表现出平坦的形态;BM样品多孔,粗糙度高)。实验处理后的表面分析与对照组相比没有表现出外貌上的差异。细胞实验结果表明,PAT处理显著增加了4种骨替代物的细胞粘附性,而UV未能显示统计学差异。细胞活力测试显示,在任何一个测试表面的巨噬细胞粘附性方面没有差异。
总之,在本研究的局限性范围内,结果表明,使用PAT处理各种骨移植材料似乎可以通过改善成骨细胞的粘附性来提高骨替代物在早期阶段的骨传导性,而不会同时影响巨噬细胞的生存能力。
原始出处:
Luigi Canullo, Tullio Genova, et al., Effects of argon plasma treatment on the osteoconductivity of bone grafting materials. Clin Oral Investig. 2020 Aug;24(8):2611-2623. doi: 10.1007/s00784-019-03119-0.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EST#
67
#骨移植#
91
#等离子体#
101
#Oral#
0