STTT:肿瘤干细胞能够产生功能性神经元支持癌症生长
2017-05-05 佚名 生物帮
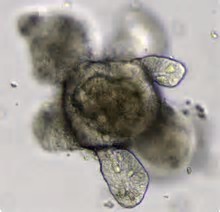
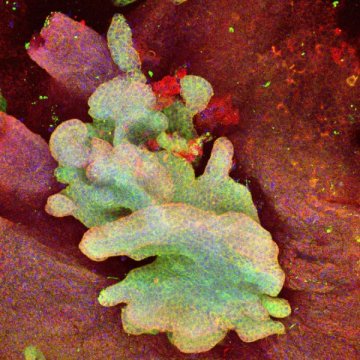
近期,国际学术权威刊物自然出版集团旗下子刊《Signal Transduction and Targeted Therapy》杂志在线发表了四川大学生物治疗国家重点实验室干细胞生物学研究室莫贤明研究组的一篇研究论文,研究证实病人胃结直肠癌干细胞能够产生功能性神经元;这些由癌细胞形成的神经元参与构成癌旁和癌组织内的神经节,支持癌症生长;团队初步在肺癌干细胞中得到相同的结果。以博士生陆然和范川文博士为
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了
62
#功能性#
34
对肿瘤的认识更进一步
67
学习了,肿瘤干细胞,肿瘤微环境
65
谢谢分享
64
没了解过这方面的内容,学习了!
49
学习了
25
增加了对肿瘤细胞的新认识
31