Cell Death Differ:NDP52突变能够促进线粒体自噬并抑制多发性硬化症中的炎症反应
2021-03-28 xiaozeng MedSci原创
多发性硬化症(MS)是一种自身免疫性疾病,其能够引起中枢神经系统的慢性炎症反应,导致脱髓鞘和轴突的损伤,最终导致运动、感觉和认知的丧失。
多发性硬化症(MS)是一种自身免疫性疾病,其能够引起中枢神经系统的慢性炎症反应,导致脱髓鞘和轴突的损伤,最终导致运动、感觉和认知的丧失。
既往研究显示,多发性硬化症是一种与线粒体功能异常有关的疾病,而线粒体自噬作用在MS中的作用仍然未知。
炎症反应过程的原因目前尚不清楚,相关理论研究显示其涉及多种因素,包括疾病的遗传易感性和能够刺激免疫系统并触发自身免疫反应的环境因素。
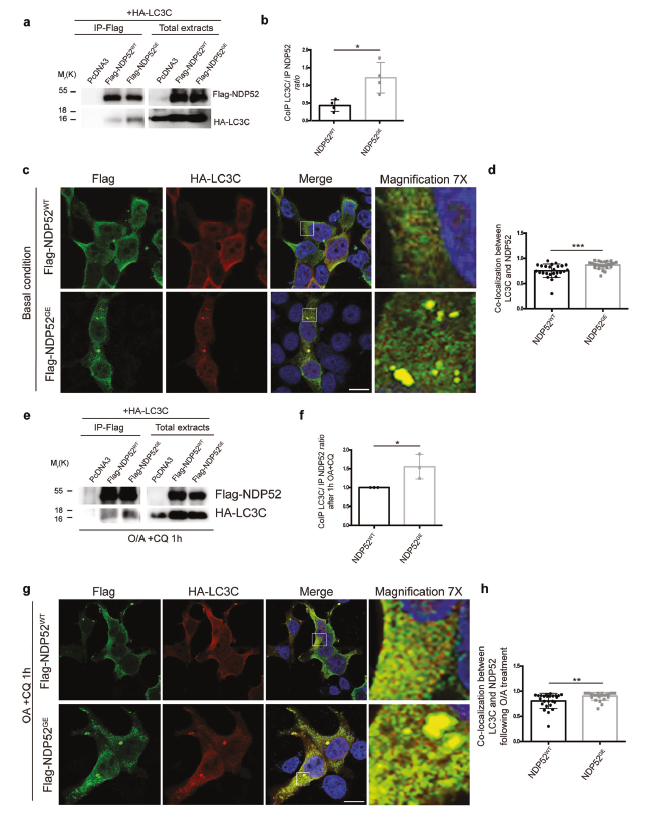
NDP52 G140E突变增加了NDP52/LC3C的结合作用
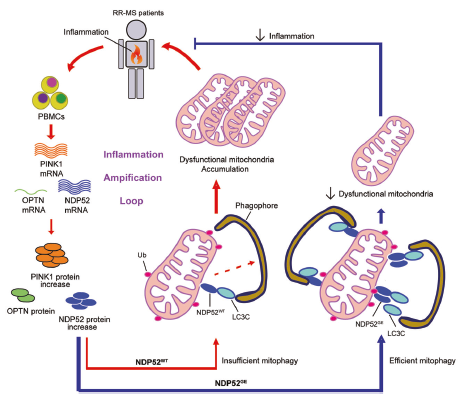
在该研究中,研究人员通过定性和定量研究,分析复发缓解型MS患者的外周血单核细胞(PBMC)中PINK1介导的线粒体自噬作用。研究人员发现,NDP52的突变体c.491G> A(rs550510,p.G140E)是主要的线粒体受体基因之一,且与MS相关。
相关机制示意图
通过研究此突变体,研究人员发现人源NDP52的第140位氨基酸残基能够调节NDP52/LC3C的结合作用,促进自噬体的形成以驱动有效的线粒体自噬作用。此外,在PBMC中,NDP52主要在B细胞中表达,并确保有效的线粒体吞噬作用,其能够限制细胞刺激后促炎性细胞因子TNF-α的产生。
总而言之,该研究结果有助于更好地理解NDP52在线粒体自噬中的作用,并揭示了其在MS中的潜在作用。
原始出处:
Di Rita, A., Angelini, D.F., Maiorino, T. et al. Characterization of a natural variant of human NDP52 and its functional consequences on mitophagy. Cell Death Differ (15 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#硬化症#
63
#CEL#
66
#Differ#
60
#多发性#
58
#Cell#
53
已读,这种事受益匪浅呀!
88
#炎症反应#
57
#Death#
51
好文章!
0