BMJ发布Meta分析:这么多COVID-19临床试验,或可降低死亡率的药物只发现了糖皮质激素
2020-08-07 医咖会 医咖会
近日,BMJ刊登了一篇文章,对COVID-19药物治疗的临床试验进行了实时系统评价(living systematic review)和网状Meta分析(network meta-analysis)。
近日,BMJ刊登了一篇文章,对COVID-19药物治疗的临床试验进行了实时系统评价(living systematic review)和网状Meta分析(network meta-analysis)。数据来自美国CDC的COVID-19数据库(包含25个电子数据库)和6个中文数据库,检索日期截止到2020年7月20日。
原文链接:
https://www.bmj.com/content/370/bmj.m2980
在对7285篇文章的标题和摘要以及122篇文章的全文进行筛选后,研究人员确认了截止到2020年7月20日的32项评估药物疗效的独立RCT研究(图1)。

图1 研究筛选过程
18项RCT的结果已经发表在同行评审的期刊上,14项仅在预印本平台上发布。大多数试验都注册过(30/32;94%)、用英文发表(30/32,94%)、针对COVID-19住院患者(28/32,88%)。超过一半的试验是在中国进行的(18/32,56%)。
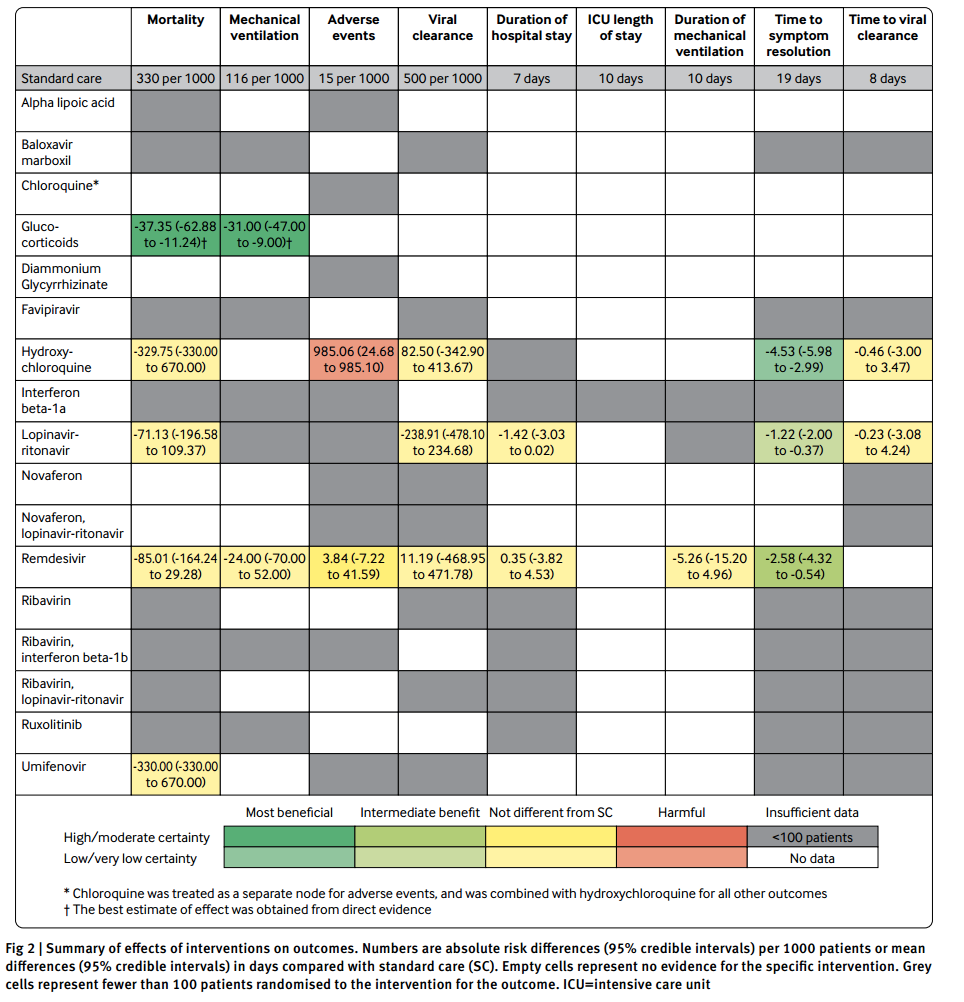
图2. 一表总结不同药物对不同结局的疗效
死亡率
15项RCT(共包含8654名参与者)报告了死亡率结局。网状Meta分析中纳入的干预措施包括糖皮质激素、羟氯喹、洛匹那韦-利托那韦、瑞德西韦、阿比朵尔和标准治疗。
结果显示,这些干预措施与标准治疗相比,并没有显示出对死亡率的明显益处。瑞德西韦对比标准治疗的研究证据确定性低,其他药物的证据确定性极低(图2)。
对于糖皮质激素,直接估计比网状估计的可信度更高。糖皮质激素对比标准治疗的两项试验的成对Meta分析(pairwise meta-analysis)表明,糖皮质激素治疗可能降低死亡率(RR 0.88[95%CI 0.80-0.97]),偏倚风险为中等。
机械通气
8项RCT(共包含6953名参与者)报告了在基线时未接受机械通气的参与者在治疗期间接受机械通气的比例。Meta分析中纳入的干预措施包括糖皮质激素、瑞德西韦和标准治疗(图2)。
糖皮质激素与标准治疗比较的成对Meta分析的证据确定性较高,结果表明糖皮质激素可降低机械通气率(RR 0.74[95%CI 0.59-0.93]),偏倚风险为中等。
3天、7天病毒清除率
10项RCT(共包含856名参与者)检测了病毒清除率。Meta分析中纳入的干预措施为羟氯喹、洛匹那韦-利托那韦、瑞德西韦和标准治疗。
没有确切证据表明哪一药物可以改善病毒清除率(图2)。瑞德西韦对比标准治疗的研究证据确定性低,其他药物比较的研究证据确定性极低。
住院时长
8项RCT(共855名参与者)报告了住院时长。Meta分析中纳入的干预措施为洛匹那韦-利托那韦、瑞德西韦和标准治疗。
接受洛匹那韦-利托那韦治疗患者的住院天数比接受标准治疗的患者少,但差异没有统计学意义(图2)。瑞德西韦看起来并没有减少住院时间。
至症状改善的时间
13项RCT(共2282名参与者)报告了至症状改善的时间。至少100名患者接受了羟氯喹、洛匹那韦-利托那韦、瑞德西韦和标准治疗。
相比标准治疗,接受瑞德西韦(平均差异-2.58天,95%CI -4.32 to -0.54,证据中等)、羟氯喹(-4.53天,-5.98 to -2.99,证据确定性低)和洛匹那韦-利托那韦(-1.22天,-2.00 to -0.37,证据确定性低)治疗的患者,症状持续时间缩短。
结论
本研究表明,糖皮质激素可能会降低COVID-19重症患者的死亡率和机械通气率。目前,大多数药物的疗效尚不确定,众多干预措施对于不同结局也缺乏确凿证据表明是有益处或者有危害。
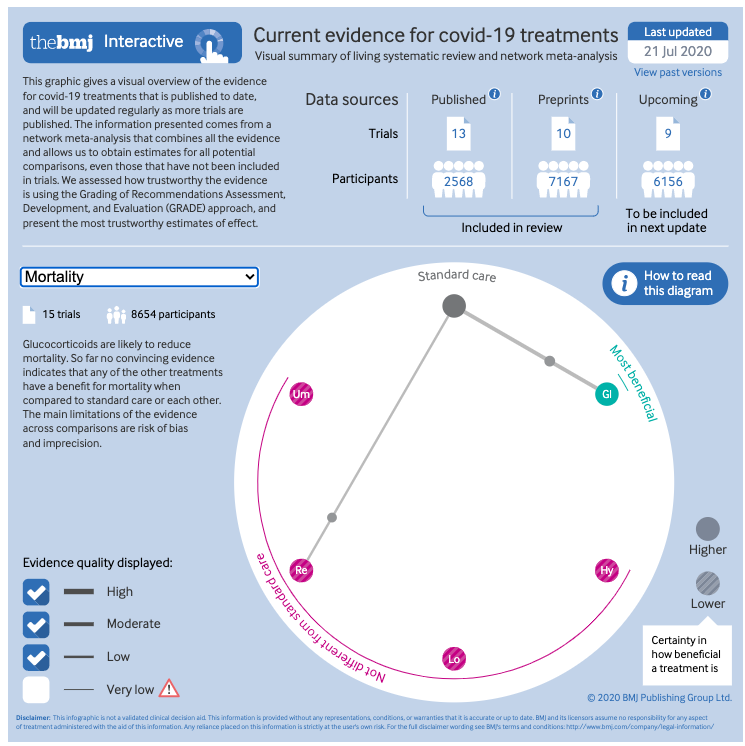
BMJ对这些证据做了交互性可视化展示,感兴趣的伙伴可以查看原文:
https://www.bmj.com/content/370/bmj.m2980
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Meta#
64
#BMJ#
54
#糖皮质#
63
#MET#
50
#皮质激素#
62