超声诊断胆囊憩室并胆汁淤积1例
2019-02-19 吴克钻 黄碧华 陈惠萍 中国超声医学杂志
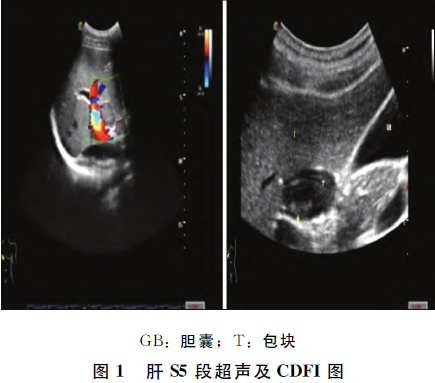
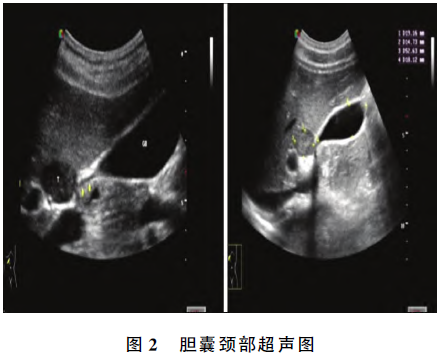
患者男,19岁。于他院超声发现肝脏占位性病变2个月余,但无不适主诉。超声检查:于肝S5段探及一低回声包块,大小29mm×17mm,边界清晰,形态规则,CDFI:包块未见明显血流信号;餐后胆嚢,显示不清。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#胆汁淤积#
90
#憩室#
80
#超声诊断#
73
#超声诊断#
0
#胆汁#
88