Ann Phys Rehabil Med: 五次重复坐站试验对慢性阻塞性肺疾病患者死亡率的预后价值
2022-06-27 xuyihan MedSci原创
慢阻肺一般指慢性阻塞性肺疾病。 慢性阻塞性肺疾病是一种具有气流阻塞特征的慢性支气管炎和(或)肺气肿,可进一步发展为肺心病和呼吸衰竭的常见慢性疾病。
慢性阻塞性肺病(COPD) 是导致过早死亡的主要原因之一, 6分钟步行试验 (6MWT)、心率、纤维蛋白原和 C反应蛋白水平以及白细胞计数已被确定为COPD患者的预后因素。尽管从临床的角度来看,许多 COPD 患者患有肌肉骨骼疾病,但很少有研究检查肌肉骨骼和功能能力测试与 COPD 死亡率之间的关联。本研究的目的是在调整现有和混杂的预后因素后,评估五次重复坐站试验在预测 COPD 患者死亡风险方面的预后价值。

本项研究是一项前瞻性和纵向研究。2014年研究人员从西班牙的一家医院招募了 137 名处于稳定期的COPD患者(平均年龄 67岁;87%为男性),并随访 5 年(2014-2019 年)。主要观察的结局指标为 5年全因死亡率,并进行了统计学分析。
研究结果显示5年内共有37名患者死亡。在 Cox 比例风险回归模型中,所有肌肉骨骼测试都与5年全因死亡率相关。然而,在调整心脏病史、既往病史后,只有五次重复坐站测试 (5-STS) 评分是严重恶化和呼吸困难的独立的预后因素(风险比为 1.04,95% 置信区间为 1.01-1.08)。该测试表现出与 6MWT 相似的5年死亡率判别能力(受试者工作特征曲线下面积:0.741 VS 0.722;p = 0.92),以及用于鉴别的高度预后截止(15.98 s)。该截止值具有比 6MWT 截止值 (~350 m) 更高的似然比 (LRs),预测效果更好。
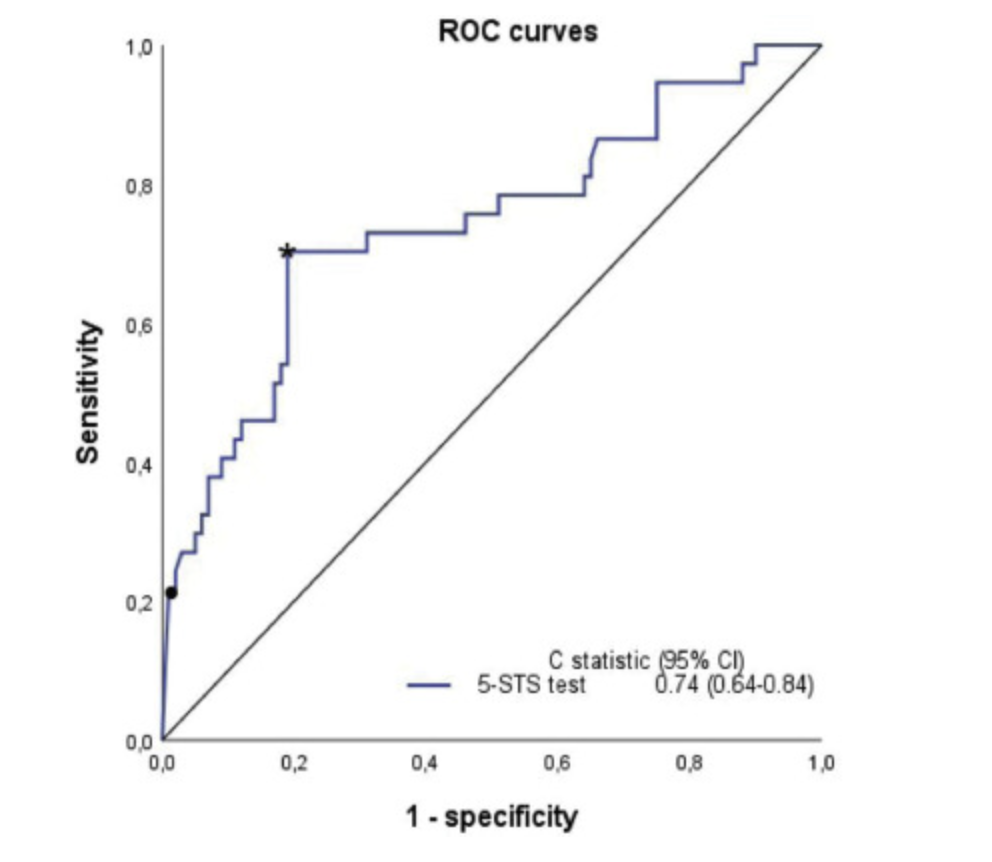
图:五次重复坐站测试 (5-STS)的预测价值
五次重复坐站测试(5-STS)是预测COPD患者死亡率的客观指标,具有良好的判别能力,判别生存率的临界值略优于6MWT。
原始出处:
FrancescMedina-Mirapeixa. Et al. Prognostic value of the five-repetition sit-to-stand test for mortality in people with chronic obstructive pulmonary disease. Annals of Physical and Rehabilitation Medicine.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者死亡#
78
#阻塞#
83
#疾病患者#
55
1
61
#预后价值#
90
#EHA#
67
#Med#
47