葛均波院士:2021年心血管治疗领域重大研究盘点
2021-12-18 心血管健康联盟信息平台 心血管健康联盟信息平台
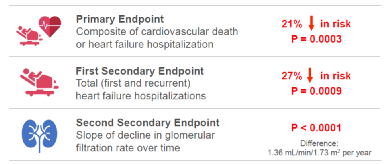
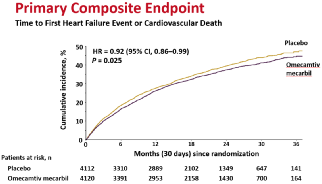
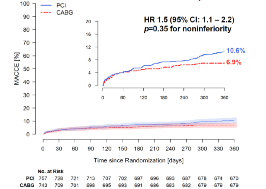
在即将过去的2021年里,心血管领域陆续公布和发表了多项重磅研究,一睹为快!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#葛均波#
170
#心血管治疗#
137
#重大研究#
146
学习
159
学习到了!!!!
150
#葛均波院士#
153
学习
156
学习
158
学习一下真不错
151
学习了!
141