Cell Stem Cell:揭示紫外线诱发皮肤癌的分子机制
2017-10-23 Hyeongsun Moon “细胞”微信号
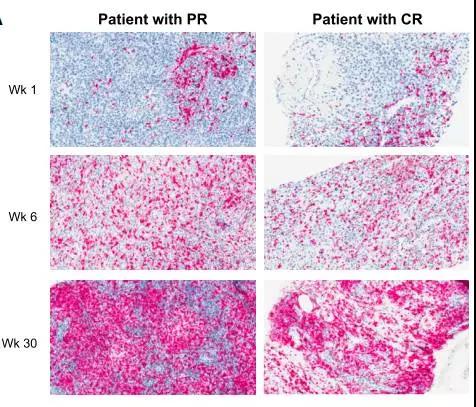
近日,一项刊登在国际杂志Cell Stem Cell上的研究报告中,来自康奈尔大学兽医学院的研究人员通过研究发现,当黑色素干细胞积累足够数量的基因突变时,其就会转变成癌症起源的细胞;在正常情况下,来自太阳光的紫外线照射(UV)会激活黑色素细胞释放黑素,黑素是一种能够保护皮肤免于太阳光晒伤的色素;但如果黑色素干细胞中积累的基因突变超过一定阈值时,当被日照所激活时就会引发肿瘤产生并生长。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
0
#Cell#
75
#stem cell#
71
#STEM#
100