电脑族必备:3套小动作预防肩周炎
2016-02-24 王春玲 上班族每日健康
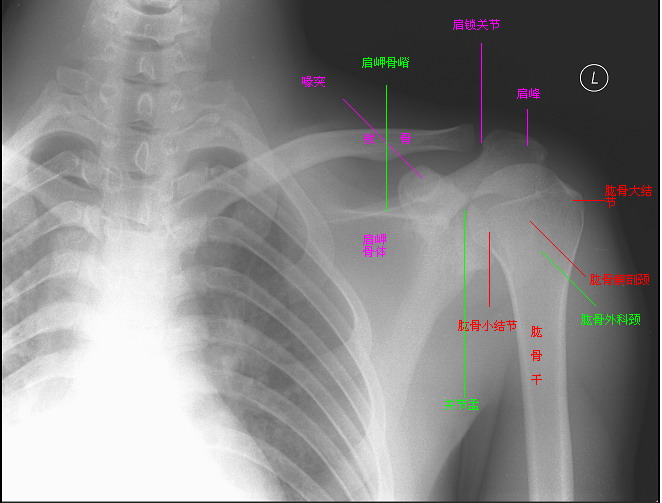
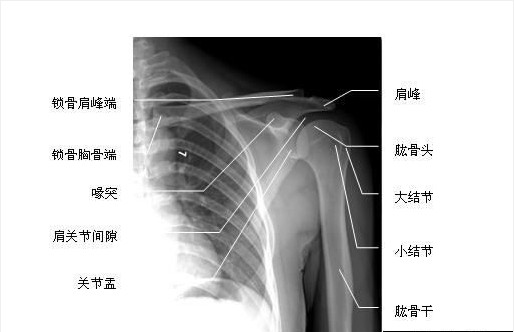
我们知道,人体骨骼之间是由光滑柔韧的结缔组织连接起来的,该部位被称为关节囊,保证了我们可以自由灵活地做出各种动作。而连接肩胛骨和肱骨的肩关节囊相对松而薄,随着机体的老化,很容易出现炎症或纤维化病变,这就是所谓的肩周炎。研究显示,肩周炎在 人群中的患病率为2% ~5%,且多发于40 ~65 岁年龄段人群,女性高于男性(60∶40)。随着久坐生活方式的日益普遍,肩周炎的发病呈现年轻化的趋势。根据症状的
我们知道,人体骨骼之间是由光滑柔韧的结缔组织连接起来的,该部位被称为关节囊,保证了我们可以自由灵活地做出各种动作。而连接肩胛骨和肱骨的肩关节囊相对松而薄,随着机体的老化,很容易出现炎症或纤维化病变,这就是所谓的肩周炎。研究显示,肩周炎在 人群中的患病率为2% ~5%,且多发于40 ~65 岁年龄段人群,女性高于男性(60∶40)。随着久坐生活方式的日益普遍,肩周炎的发病呈现年轻化的趋势。根据症状的不同,肩周炎的发病过程大致可分为四个阶段:第一个阶段被称为粘连前期(preadhesivestage)或炎症期(inflammatorystage),主要表现为肩部疼痛感逐渐加剧,但活动尚不受限,该阶段一般会持续10~12周;第二个阶段被称为渐冻期(freezing stage),主要表现为高度的疼痛感,活动已逐渐受限,大幅度的抬臂或扭臂动作已无法完成,该阶段大约会从发病第10周持续到第36周;第三个阶段被称为僵硬期(frozenstage),临床表现为疼痛感开始缓解,但活动能力大幅受限,特别是肩外旋、内旋和外展活动度全面下降,这一症状大致会从发病第36周持续至第52周;随后病症进入缓解期(thawing stage),疼痛感逐渐消失,活动度逐渐恢复。因此肩周炎具有自限性的特点,也就是病症在发生发展到一定程度后能自动停止,并逐渐恢复。一般未经治疗患者的整个病程为12~42个月,平均为30个月。但是即使病情得到了最大程度的恢复,仍有约六成的患者不 能完全恢复正常,患病肩部的活动度明显低于对侧正常肩关节。
因此,尽管在多数情况下肩周炎是可以不治而愈的,但为了减少长期的病痛折磨,避免活动力减退,采取适当的治疗手段是十分必要的。目前对于肩周炎的治疗大致分为保守治疗和手术治疗两大类。其中保守治疗包括药物治疗和物理治疗。常见的药物有非甾体类消炎镇
痛药以及可的松等激素类药剂,然而这些药物一方面疗效有限,大多仅适用于病痛早期,同时可能会产生副作用,对机体造成不必要的损伤。相比之下,康复性练习和拉伸按摩等物理性治疗手段更加安全有效,尤其对处于病程第二和第三阶段的患者更为适用。这里要特别指出的是,按摩是一个专业性很强的操作,手法不当可能会引发骨折、关节脱位、肩袖损伤、臂丛神经损伤、关节周围软组织损伤等严重后果,因此应到专业的医疗机构就诊,不要随意自行按摩。对于重症患者更需要及时就医,必要时可接受关节镜微创手术治疗。
对于上班族来说,长久伏案工作也是诱发肩周炎的重要因素。最好的预防方法就是养成良好的坐姿,并且有意识地定时起身做些小运动。美国整形外科医师协会(AmericanAcademy ofOrthopaedicSurgeons)针对久坐人群给出了一套可有效预防肩周炎的运动方案,如下文所述。
①转体训练:在门边站立,手指握住门框,小臂呈水平状态。转体90°并保持该状态30秒。放松,换另一侧并反复数次。
②上臂前举训练:双腿伸直仰卧于垫子上。左手托住右肘将右臂举过头顶,直至感到轻微拉伸感,保持15秒。缓慢放下手臂。放松,换另一侧并反复数次。
③双臂交叉拉伸训练:上体直立,左手扶住右肘,在不引起疼痛 的前提下,尽可能地向胸前拉伸,保持30秒。放松,换另一侧并反复数次。
所以说,对于肩负工作和生活重任的我们,在紧张忙碌之余,要多给自己的肩膀一些关爱,让我们更有力量去迎接一个又一个挑战。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












是的多学习原来如此
169
动起来
202
值得学习
199
赞
147
边看边学
205
正在家里做
176
收下
142
收藏
171
不错不错
205
推荐
159