肝脏也会自相残杀?聊聊自身免疫性肝病那些事儿
2016-07-20 丁敬献 赵洪礼 东省消化病防治中心 医学界消化频道
在临床工作中常有一些病因不明、肝功能反复异常的肝病患者,难以明确诊断并给予相应治疗,给临床医师带来较大的困惑,患者亦承受严重的心理和经济负担。这部分患者往往在完善了相关检查,且排除了细菌、病毒、药物、酒精、寄生虫、代谢因素造成的肝脏损害后,仍不能明确诊断的,应高度警惕自身免疫性肝炎。自身免疫性肝炎(Autoimmune Hepatitis,AIH)为自身免疫反应介导的慢性进行性肝脏炎症性疾病,
在临床工作中常有一些病因不明、肝功能反复异常的肝病患者,难以明确诊断并给予相应治疗,给临床医师带来较大的困惑,患者亦承受严重的心理和经济负担。这部分患者往往在完善了相关检查,且排除了细菌、病毒、药物、酒精、寄生虫、代谢因素造成的肝脏损害后,仍不能明确诊断的,应高度警惕自身免疫性肝炎。
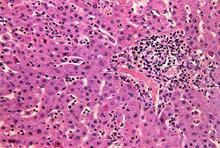
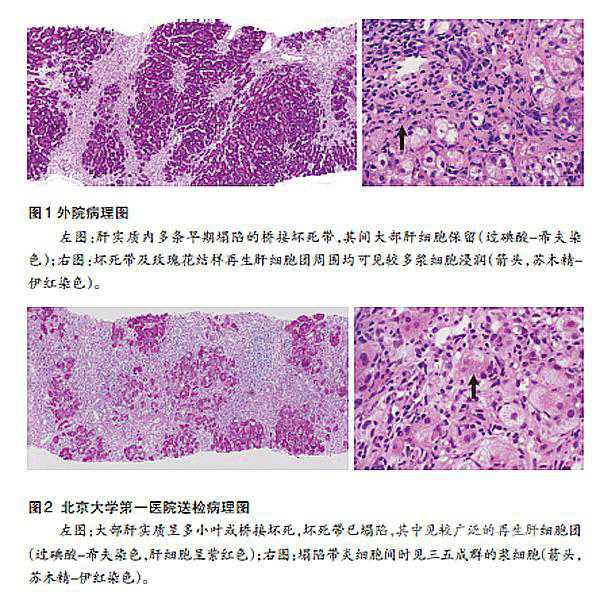
自身免疫性肝炎(Autoimmune Hepatitis,AIH)为自身免疫反应介导的慢性进行性肝脏炎症性疾病,是一种由针对肝细胞的自身免疫反应所介导的肝脏实质炎症,以血清自身抗体阳性、高免疫球蛋白G( IgG) 和( 或) γ-球蛋白血症、肝组织学上存在界面性肝炎为特点,如不治疗常可导致肝硬化、肝衰竭。本病为遗传倾向疾病,具备易患基因的人群可在环境、药物、感染等因素激发下起病。
一、诊断
(一)、实验室检查
1.转氨酶活性:主要表现为肝细胞损伤型改变,AST和ALT活性升高,而ALP和GGT水平正常或轻微升高。病情严重或急性发作时血清TBil水平可显著升高。ALT常高于正常值10倍以上,ALT高于AST。血清胆红素水平中度升高。自身免疫性肝炎典型的表现是突出的高丙种球蛋白血症。85%AIH患者血清γ-球蛋白和免疫球蛋白IgG水平升高。血清IgA升高者,相较于AIH更应考虑脂肪性肝炎(酒精性或非酒精性)或药物性肝损的诊断。此外血清IgM升高则是原发性胆汁性肝硬化(PBC)的特征性指标。
2.免疫血清学检查:多种自身抗体阳性为本病的特征。(1)抗核抗体(ANA)80%的患者体内有此抗体,其滴度和血清7-球蛋白水平相一致。(2)平滑肌抗体(SMA)约70%病例阳性,为IgM,其抗原和平滑肌与骨骼肌的S肌动蛋白有关,也存在于肝细胞膜和细胞骨架的收缩成分,因而SMA也可看做是肝细胞损坏的结果。(3)可溶性肝抗原抗体(抗-SLA)为针对一种可溶性肝抗原的非器官特异性抗体,主要存在于年轻女性病例中,这类患者对类固醇激素治疗反应良好。(4)抗肝-肾微粒体抗体(LKM),是Ⅱ型AIH的主要特征。 (5)线粒体抗体(AMA)30%的病例阳性。
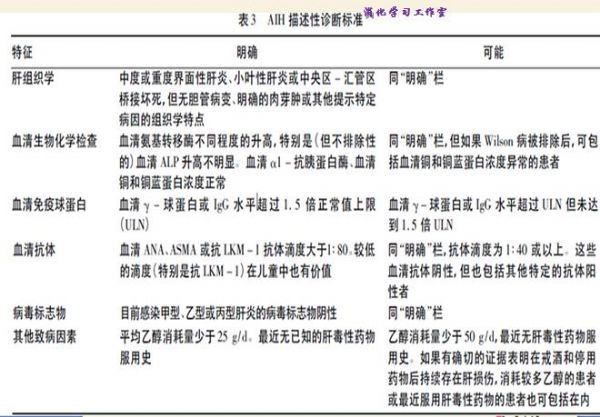
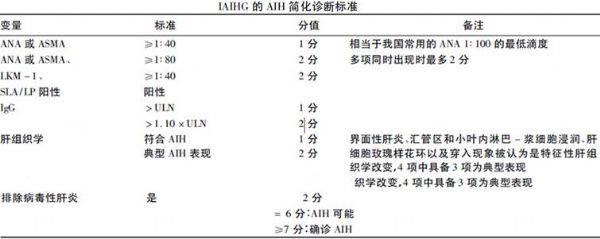
(二)AIH的一般诊断标准
1.主要标准:(l)高γ-Gl血症或IgG升至2g/dl以上。(2)肝炎病毒标志(如HBV、HCV等)阴性(偶伴有HCV血症或病毒既往感染标志)。(3)血中自身抗体(ANA、SMA、SLA、LKM、ASGPR)阳性。特别是ANA与SMA。(4) HLA-B8、DR3、DR4阳性。(5)肝组织学证据(肝脏活检在诊断AIH方面具有重要意义,是确认疾病完全缓解以及明确理想治疗终点的唯一方法。)
2.辅助标准:(l)中年以下女性好发。(2)常伴有自身免疫疾病的发病特点或有关疾病。(3)关节痛。(4)血清转氨酶持续或反复性升高。 (5)除外酒精性、药物性、代谢性等其他肝病。凡符合1-4项主要标准者可考虑AIH,进一步做肝组织学检查。若符合全部5项主要标准则可确诊。
二、临床表现
AIH 临床表现多样,大多数AIH患者起病隐匿,一般表现为慢性肝病。最常见的症状包括嗜睡、乏力、全身不适等。体检可发现肝大、脾大、腹水等体征,偶见周围性水肿。约1/3 患者诊断时已存在肝硬化表现。10% - 20% 的患者没有明显症状,仅在体检时意外发现血清氨基转移酶水平升高。这些无症状患者进展至肝硬化的危险性与有症状患者相近。AIH 可在女性妊娠期或产后首次发病,早期诊断和及时处理对于母婴安全非常重要。约25%的AIH 患者表现为急性发作,甚至可进展至急性肝衰竭。部分患者AIH 病情可呈波动性或间歇性发作,临床和生物化学异常可自行缓解,甚至在一段时间内完全恢复,但之后又会复燃。这种情况需引起高度重视,因为这些患者的肝组织学仍表现为慢性炎症的持续活动,不及时处理可进展至肝纤维化。
三、治疗
AIH 治疗的总体目标是获得肝组织学缓解、防止肝纤维化的发展和肝衰竭的发生,延长患者的生存期和提高患者的生存质量。临床上可行的治疗目标是获得完全生物化学指标缓解,即血清氨基转移酶( ALT/AST) 和IgG 水平均恢复正常。
1.治疗指征
所有活动性AIH 患者均应接受免疫抑制治疗,并可根据疾病活动度调整治疗方案和药物剂量。
1.1 中度以上炎症活动的AIH 患者(血清氨基转移酶水平>3×ULN、IgG >1.5×ULN),急性{ALT 和( 或) AST>10×ULN}甚至重症{伴出凝血异常: 国际标准化比值(INR)>1.5}应及时启动免疫抑制治疗,以免出现急性肝衰竭。
1.2 对于轻微炎症活动( 血清氨基转移酶水平<3×ULN、IgG< 1.5×ULN)的老年(>65岁)患者需平衡免疫抑制治疗的益处和风险作个体化处理。暂不启动免疫抑制治疗者需严密观察,如患者出现明显的临床症状,或出现明显炎症活动可进行治疗。
1.3 从肝组织学角度判断,存在中度以上界面性肝炎是治疗的重要指征。轻度界面性肝炎的老年患者可严密观察、暂缓用药,特别是存在免疫抑制剂禁忌证者。而存在轻度界面炎的年轻患者仍有进展至肝硬化的风险,可酌情启动免疫抑制治疗。对非活动性肝硬化AIH 患者则无需免疫抑制治疗,但应长期密切随访( 如每隔3 -6 个月随访1次)。
2.治疗方案
自身免疫性肝炎的治疗原则主要是抑制异常的自身免疫反应,治疗指征主要根据炎症活动程度,而非肝功能受损程度。如若病人出现症状明显,病情进展快或γ球蛋白≥正常值的2倍,以及谷草转氨酶≥正常值5倍、谷丙转氨酶≥正常值10倍等情况时,可考虑使用皮质类固醇治疗。经使用免疫抑制剂治疗后,65%的病人可获得临床、生化和组织学缓解。有肝硬化和无肝硬化病人10年生存率分别为89%和90%,因此,有必要严格规范用药。
(1)单用强的松疗法适合于白细胞明显减少、妊娠、伴发肿瘤或硫嘌呤甲基转移酶缺陷者,或仅需短程治疗者(≤6个月)。第一周:强的松60 mg/d;第二周:40 mg/d;第三周:30 mg/d;第四周:30 mg/d;第五周起:20 mg/d,维持到治疗终点。
(2)强的松与硫唑嘌呤联合疗法适用于绝经后妇女、骨质疏松、脆性糖尿病、肥胖、痤疮、心理不稳定或有高血压者。强的松剂量为第一周:30 mg/d;第二周:20 mg/d;第三周:15 mg/d;第四周:15 mg/d;第五周起:10 mg/d。第一周开始即同时服用硫唑嘌呤50 mg/d,维持到治疗终点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










好文章,受益
78
赞一个!好文章拜读了,认真学习了。
65
好文章,值得学习,先赞一个
88
#自身免疫性肝病#
40
学习,好文章,很实际用途
138
学习学习!
112
好文章
57
值得阅读
97
继续学习
90
继续关注
53