J Clin Oncol:局部晚期NSCLC术后应该先放疗还是先化疗?
2017-12-24 Wrangx 肿瘤资讯
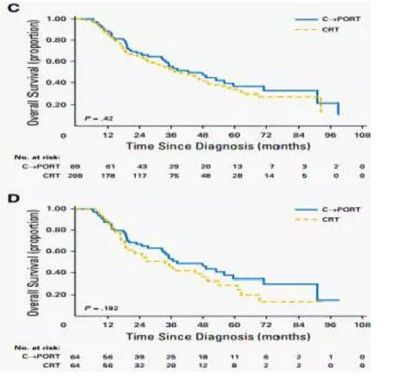
对于完全切除的pN2期或不完全切除的局部晚期NSCLC,术后化疗和放疗是同步还是序贯还存在争议。2017年12月13日JCO在线文章发现对于R0切除pN2患者先化疗再放疗较同步放化疗改善生存。对于术后切缘阳性患者放化疗顺序与生存改善无关。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
84
#局部晚期#
80
学习了.谢谢分享
128
学习并分享!!
111
一起学习
120
#局部#
75
#晚期NSCLC#
71
学习了.谢谢分享
107
很有价值
116
不错的文章值得推荐
70