Science&Cell Host & Microbe :两篇重磅揭示结肠癌与肠道菌群的关系!肠道菌群竟可致癌!
2018-02-05 Yui 转化医学网
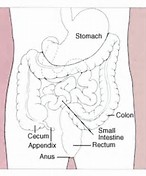
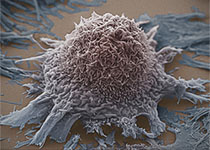
结直肠癌(CRC)是最常见的恶性肿瘤,由通过促进正常粘膜向腺癌转变的结肠上皮细胞(CEC)突变的积累而发展。大约5%的CRC发生在具有遗传突变的个体中。最近的一项研究发现肠道内的两种细菌可能与结直肠癌的发病有关。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Micro#
88
#Cell#
81
#CEL#
91
可以扩宽临床研究.好文章
108
学习
0
好
141
#CRO#
64
好
107
好
122
太好了
107