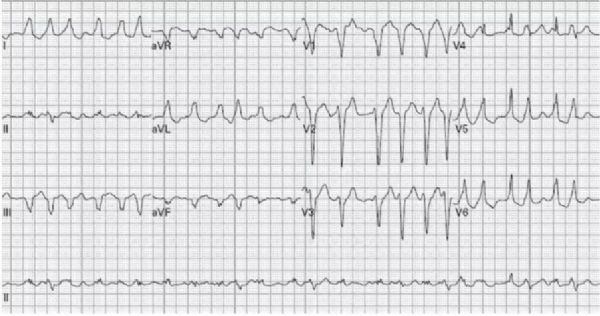
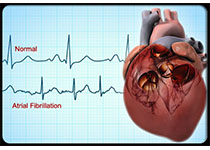
病例分享:房颤伴预激?多形性室速?房颤并发差异性传导?
2018-02-12 江苏省人民医院 卢妙 许迪 黄元铸 中国医学论坛报今日循环
1例53岁女性患者,心悸伴头晕半小时,心电图如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



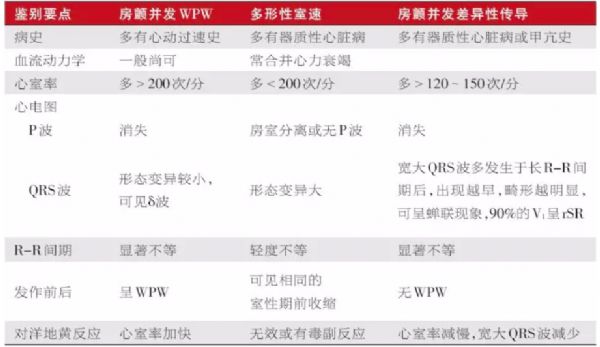






#并发#
94
#多形性#
91
学习一下谢谢
99
#室速#
84
学习一下谢谢
92