病例分享:心脏手术2年多,反复伤口渗脓和面部皮疹为哪般?
2018-01-29 黄英男 金文婷 马玉燕 SIFIC感染官微
主诉:心脏术后切口反复渗脓伴面部皮疹2年余
一、病史简介
女性,58岁,浙江人,2017-12-11入中山医院感染病科
主诉:心脏术后切口反复渗脓伴面部皮疹2年余
现病史:
2015-08因“风心二尖瓣狭窄伴关闭不全,冠心病三支病变”在外院行二尖瓣机械瓣换瓣术+冠脉搭桥术。2016-05起手术切口中下段红肿渗脓。2016-06超声:胸部正中切口皮下液性暗区(约4.3X0.9cm),予创面换药无明显好转。2016-09-23于原手术医院行胸部伤口探查+清创:胸部伤口中段可见两个小瘘口,瘘口内部可探及胸骨固定钢丝,取出钢丝2根,充分清除感染组织。术后拆线时见切口底部有中量脓液渗出,继续换药治疗。2017-01再次行胸壁清创术,取出剩余1根钢丝。2017-02切口中下部两处窦口形成伴少量脓液渗出。
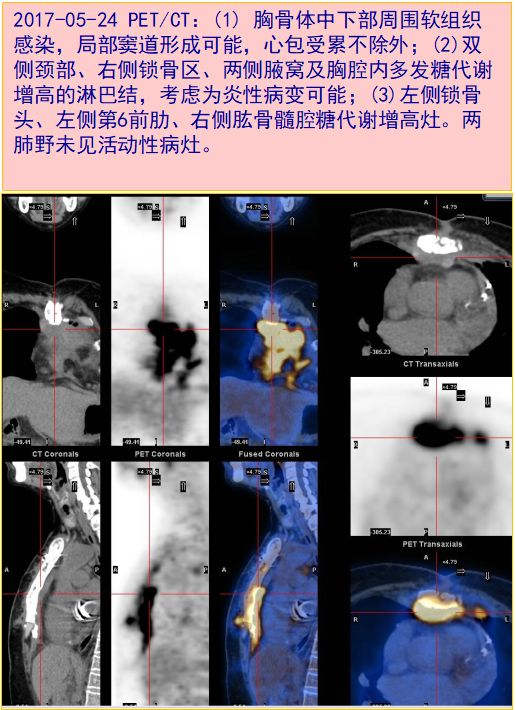
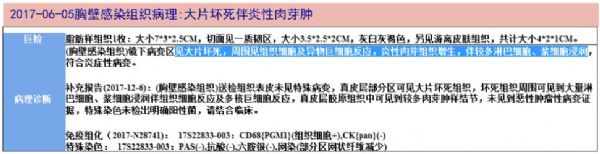
2017-05-24就诊我院整形外科,行PET/CT显示,(1) 胸骨体中下部周围软组织感染,局部窦道形成可能,心包受累不除外;(2)双侧颈部、右侧锁骨区、两侧腋窝及胸腔内多发糖代谢增高的淋巴结,考虑为炎性病变可能;(3)左侧锁骨头、左侧第6前肋、右侧肱骨髓腔糖代谢增高灶。心超:人工机械二尖瓣未见明显异常。05-25送伤口脓液细菌培养:阴性。05-31起予左氧氟沙星抗感染治疗。06-02行胸骨及前纵隔感染清创+肌瓣转移+皮瓣转移。病理:(胸壁感染组织)见大片坏死,周围见组织细胞及异物巨细胞反应,炎性肉芽组织增生,伴较多淋巴细胞、浆细胞浸润,特殊染色未检出明确阳性菌。06-12出院并继续左氧氟沙星抗感染16天。
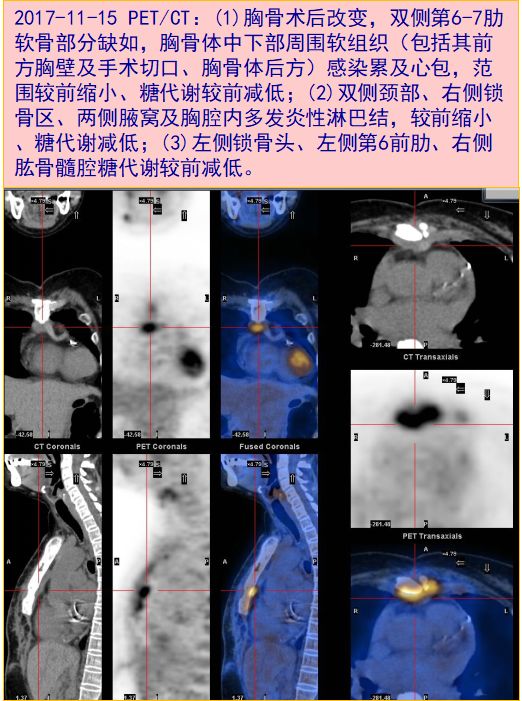
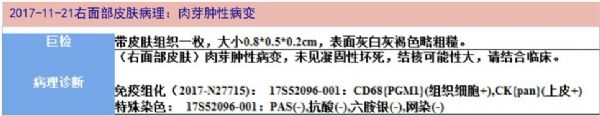
2017-11因再次出现胸部手术切口渗脓入住我院整形科。同时,患者诉2015-11起无明显诱因出现右颊部多枚丘疹样皮疹,起初范围较小,约1cm直径,无明显发红瘙痒,当地医院予药物外涂半年(具体不详),皮疹结痂。2016-05起结痂皮疹处出现水泡,伴发红,无瘙痒,范围逐渐扩大。近期面部皮疹范围进一步扩大。2017-11-14面颊皮疹处活检,病理为肉芽肿性病变,抗酸和六胺银染色均阴性。2017-11-15复查PET/CT,与05-24比较:胸骨体中下部周围软组织感染、多发炎性淋巴结、左侧锁骨头和右侧肱骨髓腔的病变范围较前缩小、糖代谢较前减低。心超同前。11-17行胸壁溃疡清创术+肌皮瓣转移术,术中见皮下组织内有一狭小窦道,内含豆渣样物。手术当天起予万古霉素抗感染7天。因感染病原体不明,为进一步诊治于12-11收治我院感染病科。
既往史个人史:20年前曾行胆囊切除术;15年前曾行阑尾切除术。
二、入院检查(2017-12-11)
体格检查:
T:36.5℃ P:86次/分 R:20次/分 BP:140/78mmHg
浅表淋巴结未及肿大。右颊可见红色成簇的丘疹,整个皮损范围约6cm直径。前胸可见长约15cm手术疤痕,局部干洁,无红肿渗出。
实验室检查:
血常规 WBC 10.05X10^9/L,N 69.3%
炎症标志物 ESR 18mm/H,CRP 11.5mg/L,PCT 0.02ng/mL
肝肾功能电解质、甲状腺功能:正常
G试验、隐球菌荚膜抗原:(-)
T-SPOT A/B:14/54
自身抗体 抗核抗体:颗粒1:100,余均(-)
肿瘤标志物:(-)
空腹血糖、糖化血糖红蛋白:正常。
三、临床分析
病史特点:患者中年女性,主要表现心脏手术2年内切口反复脓性渗液,并伴有慢性持续扩大的面部狼疮样皮疹,炎症标志物稍升高,无发热盗汗,T-SPOT阳性;PET/CT提示手术区域及附近软组织感染,以及颈部、腋下和纵膈淋巴结糖代谢增高;手术部位胸壁组织和面颊皮损处活检,均提示有肉芽肿性病变。诊断和鉴别诊断考虑如下:
1.感染性疾病:
非结核分枝杆菌(NTM)感染:心脏术后切口慢性感染,NTM是常见病原体,包括龟分枝杆菌、脓肿分枝杆菌、偶发分枝杆菌、瘰疬分枝杆菌,以及鸟-胞分枝杆菌、堪萨斯分枝杆菌等,病理常表现为肉芽肿性病变。但本例T-SPOT阳性,且斑点数较高(A和B抗原,分别为14和54),与常见NTM感染不符。当然,不排除结核和非结核分枝杆菌同时感染之可能。本病确诊有赖于分枝杆菌培养或核酸检测。
结核:患者面颊皮损持续进行性进展2年多,其形态也比较符合寻常狼疮(慢性进行性皮肤结核),结合皮肤活检和T-SPOT结果,需要怀疑皮肤结核。而同期出现的心脏手术后切口慢性感染,迁延不愈,病理也提示肉芽肿性病变,按一元论解释,则考虑结核感染可能大。但患者多次胸壁感染组织和皮肤活检组织,抗酸染色均无阳性菌发现。建议行脓液及病变组织抗酸杆菌涂片+分枝杆菌培养、核酸检测,以明确诊断。
金黄色葡萄球菌感染:金葡菌是皮肤软组织和手术切口感染的常见病原体。但金葡菌感染往往起病急,炎症标志物升高显着,伴有发热等较严重毒性症状,普通细菌培养常可分离到本菌。本例患者起病慢,病程长,炎症标记物仅稍有升高,毒性症状不明显,病理提示肉芽肿病变,故暂不考虑此诊断。
2.非感染性疾病:
患者有多处淋巴结肿大且糖代谢增高,面颊部丘疹病变等,需要考虑淋巴瘤、癌症转移、系统性红斑狼疮(SLE)等疾病,但患者胸壁坏死组织和面颊部皮损组织活检显示为肉芽肿病变,同时抗感染治疗后PET/CT显示,胸部病变范围有缩小和糖代谢下降,故此类疾病,也暂不考虑。
四、进一步检查、诊治过程和治疗反应
12-12 拟行胸骨处病灶穿刺活检术。但超声下胸骨术区未见明显脓肿形成,认为不宜穿刺。
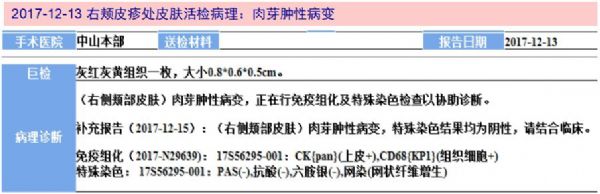
12-13 行右颊部皮疹处再次活检。活检组织送涂片找细菌、真菌、抗酸杆菌均阴性,细菌、真菌培养阴性。病理仍显示“肉芽肿性病变”。
12-14出院等待分枝杆菌培养结果再确定具体抗感染方案
2018-01-11 皮肤活检分枝杆菌培养结果:结核杆菌阳性。
2018-01-17 开始予异烟肼+利福平+乙胺丁醇+吡嗪酰胺四联抗结核治疗。
2018-01-28 面部皮疹较前明显好转。嘱继续抗结核治疗,1月后随访胸部CT。
五、最后诊断与诊断依据
最后诊断:
多部位结核病
手术切口(胸壁)、颈和胸部淋巴结、面部皮肤
诊断依据:
中年女性,心脏术后切口反复渗脓2年,同时伴有面颊皮损持续进行性进展,其形态似寻常狼疮。PET/CT提示术区及附近软组织感染,胸部感染组织及面颊皮疹处活检均提示肉芽肿性病变,结合T-SPOT阳性,抗结核治疗2周面部皮疹明显好转,尤其是皮肤活检组织培养出结核杆菌,故本病诊断可以明确。
六、经验与体会
心脏术后切口慢性化脓感染,全身毒性症状不明显,常需考虑特殊病原体感染,特别是非结核分枝杆菌(NTM)感染,通常因手术器械消毒不合格或冲洗液体污染引起。与结核病类似,病理主要为慢性炎症伴肉芽肿。早期多表现为局部疼痛,硬结肿块,脓肿形成或破溃,皮肤溃疡等。然而,本例综合分析判断为结核分枝杆菌引起,临床甚为少见。文献报道心脏术后NTM感染平均时间为1.4 ±1.1月,而结核感染时间较NTM更长,可达13.3 ±17.1月。本例手术后9个月首次出现手术切口红肿渗脓,潜伏期长,似乎更符合结核的发病特点。
该患者除手术部位结核感染外,术后出现面颊部皮疹,通常不易将两者联系起来考虑。我院感染病科开设病房两年多来,已收治肺外结核近百例,主要为淋巴结结核、腹腔/肠结核、骨关节结核、泌尿系结核等,皮肤结核则甚少遇见。本例面颊皮疹虽有一定特征性,类似寻常狼疮表现,但由于很多临床医生缺少对本例认知和警惕性,被延误诊断超过2年。活检是诊断皮肤结核的重要手段,然而本例首次活检仅显示为“肉芽肿病变”,我们建议患者再次活检,并对标本同时进行分枝杆菌培养,才得以明确诊断。值得指出的是,先前患者胸部手术切口反复渗脓,仅做一次普通细菌培养,而未做抗酸杆菌检查和分枝杆菌培养,错过了手术部位特殊感染病原体的诊断机会。
比较困惑的是,胸部手术切口结核感染、面颊皮肤结核感染、胸腔和颈部淋巴结结核感染,三者之间的关系?同时存在手术部位及远隔部位(面颊皮肤)的结核感染,这在既往文献中罕有报道。根据通常的结核发病机制,淋巴结结核系淋巴引流处组织的结核病灶扩散导致;皮肤结核的发病包括外源性接种、局部扩散或自体接种的内源性传播、以及血行播散三条路径,而本例更倾向于血行播散所致。由此推测,本例是否首先出现手术部位(胸壁)结核感染,再引发淋巴结结核,以及血性播散导致面颊皮肤结核感染?
本例手术切口感染反复渗脓,伤口时好时坏,考虑与之前使用的抗菌药物有关。多次使用的氟喹诺酮类药物,对结核杆菌有强力杀灭作用,所以治疗后能控制病情,但单药且使用时间很短,导致一段时间后结核很快复发。这里特别需要呼吁,对于疑似结核病人,一定要加强病原学检查,并早期、联合、规律、全程使用抗结核药物。切忌不规则抗痨治疗,以免快速诱导结核菌对不规则使用的药物产生耐药,显着增加今后抗结核治疗的难度和成本,甚至让结核病成为无药可用的“不治之症”。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#面部皮疹#
73
阅
98
好好好好好好好好
99
学习了很有用
115
非常好.谢谢分享
97
很好的文章.谢谢分享
103