Cell Death Dis:CtBP通过抑制DRs决定卵巢癌细胞的命运
2020-05-10 QQY MedSci原创
高级别浆液性卵巢癌(HGSOC)是一种复杂的异质性疾病,在上皮性卵巢癌中占70%,目前仍是最致命的妇科恶性肿瘤。 HGSOC的主要治疗手段为外科肿瘤细胞减灭术和化疗的联合方案。
虽然该疾病最初对化疗敏感,但大多数的HGSOC逐渐发生基因组的变异并最终出现无法治愈的疾病复发。因此,了解HGSOC增殖的遗传与分子特征可以有效的改善其治疗策略。
近期研究发现,在上皮性卵巢癌中CtBP2(C-末端结合蛋白2)的表达水平升高,尤其是在高侵袭性和高致死性的HGSOC亚型中,而且CtBP2的表达与不良预后相关。但是,HGSOC的发生发展是否依赖于CtBP2或是其旁系同源物CtBP1目前还有待研究。
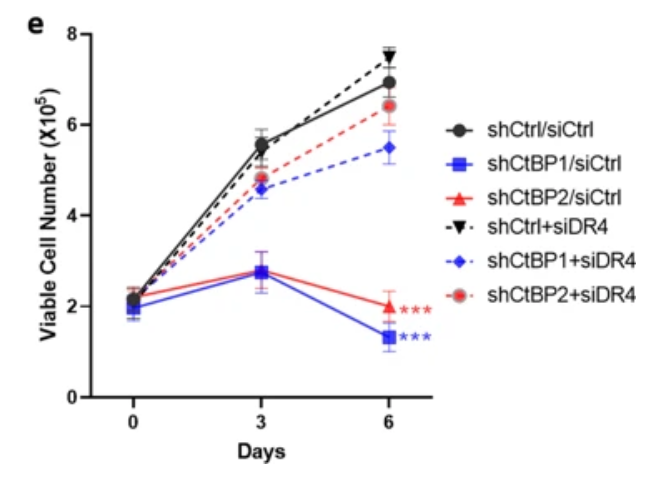
在该研究中,研究人员发现CtBP1/2可以通过沉默DR4/5抑制HGSOC的细胞凋亡过程。敲低CtBP1/2的表达水平均会上调DR4/5表达,并通过激活caspase 8引起细胞自发性凋亡。CtBP1/2缺失引起的DR4/5激活也会提高HGSOC细胞对促凋亡DR4/5配体TRAIL的敏感性。
与CtBP1/2作为转录抑制因子的功能相一致的是,其能够与DR4/5的启动子区域结合并抑制DR4/5的表达,潜在的机制可能是通过将其募集到抑制性转录调节复合物中来实现的。研究人员还发现CtBP1/2需要共同参与DR4/5的抑制作用。
总的来说,该研究发现了CtBP1/2是影响DR4/5的表达和活性的有效的抑制因子,提示CtBP或可作为HGSOC的潜在治疗靶标。
原始出处:
Ding et al. CtBP determines ovarian cancer cell fate through repression of death receptors. Cell Death and Disease (2020) 11:286
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Dis#
118
#Cell#
92
#CEL#
81
#卵巢癌细胞#
109
#癌细胞#
64
#Death#
63