Plos Medicine:可控风险因素和阿尔兹海默症的关联
2015-06-26 佚名 生物谷
全球存在大约四千万老年痴呆症患者,而且数量还有增加的趋势,据估计到2050年全球将会有1.5亿老年痴呆患者。这些老年患者往往表现为记忆力下降,交流障碍和认知功能障碍。在这些老年痴呆患者中,最常见的是阿尔兹海默症(AD),大约占到60%-70%。研究者们一直在试图寻找AD的成因,尤其是那些可能的可控风险因素,因为通过控制这些因素可能可以降低AD的发病率。流行病学的研究已经发行了几种潜在的风险因素,例
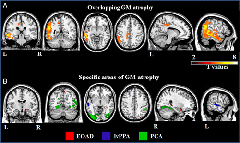
全球存在大约四千万老年痴呆症患者,而且数量还有增加的趋势,据估计到2050年全球将会有1.5亿老年痴呆患者。这些老年患者往往表现为记忆力下降,交流障碍和认知功能障碍。在这些老年痴呆患者中,最常见的是阿尔兹海默症(AD),大约占到60%-70%。研究者们一直在试图寻找AD的成因,尤其是那些可能的可控风险因素,因为通过控制这些因素可能可以降低AD的发病率。流行病学的研究已经发行了几种潜在的风险因素,例如高血压、高血脂、肥胖和吸烟等。然而,具体的相关关系或者谁为因谁为果,还是很不清楚。近期Plos Medicine发文定量讨论了这些风险因素和AD的因果关系。作者使用孟德尔遗传概率分析的方法,试图探讨了这些风险因素和阿尔兹海默症间的因果关系。
在这种孟德尔遗传概率分析法中,因果关系是通过推测不同风险因素相关的遗传突变的效应得到的。这些遗传突变体是与我们感兴趣的风险因素相关的。正是因为这些突变体是通过遗传随机获得的,它们会倾向于有序,而且它们与反向的因果关系也是无关联的。例如,我们认为高血压可能实际上会导致AD,那么那些会影响着高血压的遗传突变也会影响着AD的发病率;如果说相反地,是AD导致了高血压,那么会影响着高血压的遗传突变并不会影响AD的发病风险。
在国际阿尔兹海默基因组计划的数据库中,研究人员们分析了17008位AD患者和37154位正常老年人的基因组数据,他们重点检测了单核酸位点多态性(SNP,一种遗传突变体的形式)的发生率,来预测风险因素对AD发病的影响。研究发现,更高的动脉收缩压会导致较低的AD发病风险;吸烟的数量也与低AD发病率相关联。其他的风险因素(肥胖和高血脂)与AD的风险不明确。这个结果与流行病学研究存在冲突。
为什么高血压会引起低AD发病率呢?一种可能的原因是,这些高血压患者会接受药物治疗。这些治疗高血压的药物,很可能是导致较低AD的首要因素。因为这个研究的数据全部来自欧洲人,因此对其他族群可能需要进一步研究。研究者还提到了,因为高血压会引起心血管疾病,因此他们并不鼓励通过提高血压来降低患AD的风险。未来对于抗高血压药物对AD发病率的影响还需要深入的研究。
原始出处:
Søren D. Østergaard, Shubhabrata Mukherjee, Stephen J. Sharp et al.Associations between Potentially Modifiable Risk Factors and Alzheimer Disease: A Mendelian Randomization Study.PLOS Medicine, June 16, 2015.DOI: 10.1371/journal.pmed.1001841
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CIN#
71
#DIC#
69
期待更好更多研究
149
#阿尔兹海默#
72
#Medicine#
75
#Med#
75
到目前为止还没有一个真正意义上的老年性痴呆的风险因素未来还需要进一步的探索另外各种不同的风险因素之间的交互作用也是研究的热点。
171