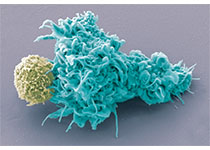
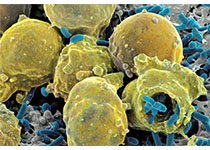
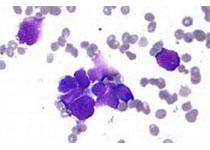
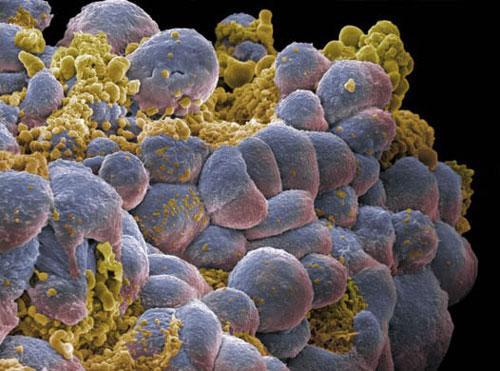
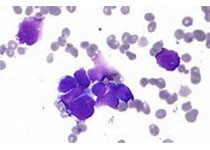
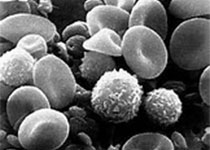
Lancet haemat:R-CHOP、放疗、利妥昔单抗维持的序贯疗法治疗晚期滤泡性淋巴瘤的效果和安全性
2018-01-25 MedSci MedSci原创
虽然目前有多种治疗方案,但晚期滤泡性淋巴瘤仍不能被治愈。而且,后诱导治疗的理想顺利和绝对优势也不清楚。现有研究人员对联合放射免疫疗法和化疗后用利妥昔单抗序贯维持治疗的效果和安全性进行评估。本研究为单臂、多中心的II期研究(SWOGS0801),从美国的20个医疗中心招募年满18岁的确诊为III-IV期或II1、II2和II3a期的既往未接受过治疗的滤泡性淋巴瘤患者。受试患者接受5年的治疗计划:R-
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HAE#
36
#序贯疗法#
43
#利妥昔#
35
#Lancet#
26
#滤泡性淋巴瘤#
37
#EMA#
25
#R-CHOP#
36