NEUROSURGERY:巨大脑动脉瘤可行搭桥术治疗
2012-12-19 NEUROSURGERY NEUROSURGERY
最新一期的《神经外科学》杂志上[Neurosurgery 2012 Nov 30]发表的的一项研究表明:对于不能行夹闭术的巨型大脑中动脉动脉瘤,颅外-颅内动脉搭桥是一项安全可行的治疗选择。 菲尼克斯圣约瑟夫医院与医疗中心,亚利桑那州Robert Spetzler教授及其研究小组称,“巨型动脉瘤进展率高,自然病程差,一旦确诊就应进行积极治疗。”但
最新一期的《神经外科学》杂志上[Neurosurgery 2012 Nov 30]发表的的一项研究表明:对于不能行夹闭术的巨型大脑中动脉动脉瘤,颅外-颅内动脉搭桥是一项安全可行的治疗选择。
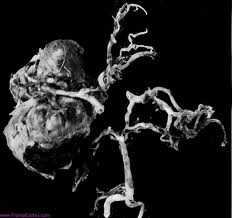
菲尼克斯圣约瑟夫医院与医疗中心,亚利桑那州Robert Spetzler教授及其研究小组称,“巨型动脉瘤进展率高,自然病程差,一旦确诊就应进行积极治疗。”但是,他们强调,由于存在动脉瘤复发可能,患者需要“终生监测”。在他们所研究的16例患者的平均58.4个月随访期间(所有动脉瘤直径均大于2.5 cm)。3例患者需再行介入治疗。在需要治疗的患者中,术后血管造影检查发现残余瘤证据者2例,行弹簧圈填塞再治疗2例,再夹闭治疗1例。再治疗未引发疾病或死亡。
Spetzler教授说,“该治疗策略背后的逻辑很简单,搭桥手术重建了动脉瘤周围区域血管,动脉瘤血流减少促进血栓形成。当血管在动脉瘤近心端结扎时,腔内压力下降,动脉瘤破裂风险降低,逆行血流减少则导致血栓形成。”
搭桥手术时,研究人员最常使用颞浅动脉进行搭桥,部分患者则采用桡动脉移植。搭桥术后,研究人员阻断载瘤血管,近心端9例,远心端4例,动脉瘤孤立术1例。
研究人员说,“在可能情况下,我们宁愿阻断近端血管,因为理论上,它在减少动脉瘤破裂风险方面占有优势。不过,当近端血流暴露受限,或动脉瘤近端部分有危险分支出现时,可选择载瘤血管远端阻断,从而导致动脉瘤栓塞和夹闭。”
手术后,除1例患者外,其余搭桥均通畅,12例患者(75%)动脉瘤完全阻断。无患者死亡,但有5例患者出现围手术期并发症,其中有症状梗死3例,分流依赖性脑积水2例。长期结果总体良好,15例患者格拉斯哥结局量表(GOS)得分为4或5。只有1例GOS得分为3,该患者因围手术期梗塞(尽管搭桥通畅)出现持续性缺血。
与脑动脉瘤相关的拓展阅读:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#搭桥#
119
#surgery#
87
#GER#
127
#ROS#
123
#搭桥术#
125
#脑动脉瘤#
149