J Arthroplasty:围术期降低全关节置换术后感染率
2014-09-12 超人也想当好医生 林超文 丁香园
在美国关节置换术是最常见的骨科手术之一。2006年美国进行约80万台全髋关节和膝关节置换手术,到2030年这个数字有可能增至400万。骨关节炎、骨缺血性坏死、炎症性关节炎和创伤后关节炎都是全关节置换术的适应症。 研究报道全髋关节置换术的感染率是0.5-1%,而全膝关节置换术是0.5-2%。假体关节感染最常见的治疗方法有移除假体、静脉注射抗生素、注入抗生素骨水泥、打入抗生素垫片、关节融合和分期修复
在美国关节置换术是最常见的骨科手术之一。2006年美国进行约80万台全髋关节和膝关节置换手术,到2030年这个数字有可能增至400万。骨关节炎、骨缺血性坏死、炎症性关节炎和创伤后关节炎都是全关节置换术的适应症。
研究报道全髋关节置换术的感染率是0.5-1%,而全膝关节置换术是0.5-2%。假体关节感染最常见的治疗方法有移除假体、静脉注射抗生素、注入抗生素骨水泥、打入抗生素垫片、关节融合和分期修复关节。由于假体关节感染的治疗费用昂贵和治疗难度高,所以预防感染就显得尤为重要。
在美国,大部分全关节置换术都是在私立医院进行的,这主要是由保险制度、患者偏好和医生水平决定的。而公立大医院的患者大多都是营养不良、静脉吸毒、酗酒,这都大大增加手术患者发生手术部位感染(SSI)的几率。CDC的研究发现私立非教学医院的术后感染率远低于教学医院,后者手术部位感染率高达8.2%。
Gottschalk医生所在的美国埃默里大学附属医院骨外科是床位超过900的一级创伤救治中心,主要接收贫穷患者或低收入患者。该院2002年到2004年间进行的70例全关节置换术的术后感染率高达12.9%。因此,Gottschalk医生设计一个详细的全关节置换术方案来降低该院手术部位感染率,文章最近发表在The Journal of Arthroplasty上。
研究纳入2002年到2003年间进行全关节置换术的70名患者作为对照组和2004年到2011年间实施新的全关节置换术方案治疗的108名患者,术后分别平均随访6.9±3.5年和2.2±2.4年。
患者个人因素与手术部位感染密切相关,如BMI/肥胖、吸烟、糖尿病、手术部位已存在感染和有MRSA定植等。因此,很多干预措施都可术前、术中或术后预防手术部位感染的发生。以下是作者所在医院2004年开始实施的全关节置换术方案:
术前处理
术前干预包括内科医师、物理治疗师、营养师、牙医和麻醉师的术前预约和评估。患者进行全关节置换术前必须完善术前相关检查。所有HIV(+)患者需接受额外的传染病检查,并且接受两种不同作用机制的抗病毒药物治疗。
另外,患者还需进行咽拭子测试观察口腔定植细菌情况,如发现咽拭子(+),则需使用7天疗程的莫匹罗星软膏。吸烟患者术前需进行尼古丁测试,阳性患者需最近两次门诊检查均阴性才能进行手术。
入院前患者需先在家用葡萄糖洗必泰液淋浴,入院后再用洗必泰擦洗手术部位。
术中处理
手术在指定手术间进行,保证房间干净和不允许感染手术或污染手术在这个房间进行。手术室通道必须保证无菌,一旦暴露关节后就不允许覆盖伤口。在患者转移至手术台前,铺上无菌单覆盖避免污染。手术医生使用洗必泰消毒。手术开始后60分钟内按患者体重打入一个单位万古霉素和头孢唑林。
首先,再用洗必泰洗刷患者皮肤;接着,浸满异丙醇的无菌巾消毒;最后,用无菌洗必泰完成手术部位洗刷。患者所有需要暴露的皮肤贴上无菌贴膜,防止皮肤表面细菌污染进入伤口。术前准备无需剃除手术部位毛发,除非毛发过多影响操作,使用电动剃刀可减少皮肤的微小创伤。
术前准备完成后,手术医生应重新更换手套。电刀只用来电凝止血,大部分操作都通过锐性分离,避免软组织发生坏死。术中应经常使用生理盐水脉冲式灌洗切口。当需要打入骨水泥假体时,把万古霉素和妥布霉素打入骨水泥假体中。
用2-0缝线或缝皮订书机缝合皮肤,再用皮肤粘合剂闭合皮肤。当粘合剂干后,用大透气胶膜覆盖伤口。1周才进行换药处理。所有患者术后都需要进行影像学检查评估假体位置。
术后管理
术后24小时内拔除导尿管。合并有多种内科疾病的患者住院期间需要在内科医生的指导下进行康复治疗。术后第1天,给予肾脏负荷剂量依诺肝素和连续压缩装置预防栓塞发生。术后24小时还需注射第Ⅳ代头孢唑林抗感染治疗。
术后可与物理治疗师和职业治疗师讨论如何进行康复治疗。如果患者需要进行社会康复服务,可由社会服务咨询师安排。
术后患者可使用自控式镇痛,术后第一天可尝试口服止痛药镇痛。住院期间,应仔细观察患者伤口渗液情况。如果术后5天,伤口渗液仍较多,患者应返回手术室进行灌洗、清创和放置引流条。
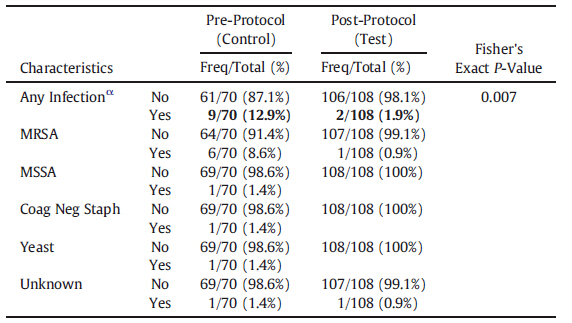
研究结果显示对照组有9名患者(12.9%)术后发生手术部位感染,其中6例MRSA感染和3例其他类型感染,而病例组只有2名患者(1.9%)术后发生感染,其中1例MRSA感染和1例其他类型感染(表1)。单变量回归分析发现病例组感染率比对照组低87%,全髋关节置换术术后感染率要比全膝关节置换术的低77%。
表1:感染类型
因此,作者认为这个新的围手术期全关节置换术管理方案可有效降低手术部位感染概率。
原始出处
Gottschalk MB1, Johnson JP2, Sadlack CK1, Mitchell PM3.Decreased infection rates following total joint arthroplasty in a large county run teaching hospital: A single surgeon's experience and possible solution.J Arthroplasty. 2014 Aug;29(8):
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#置换#
70
#AST#
94
#关节置换术#
101
#围术期#
71
#ART#
70
#全关节置换术#
115
#置换术#
75